The Biology of Reproduction - Understanding Fertility
Welcome to the fascinating world of reproduction! It's a topic that not only involves biology but touches on the very essence of life itself. When we talk about fertility, we’re diving deep into the intricate biological processes that allow for the creation of new life. Understanding fertility is crucial, whether you're planning a family, studying biology, or simply curious about how life perpetuates itself. In this article, we will explore the biological mechanisms behind fertility, the anatomy involved, and the myriad of factors that can influence conception.
Fertility is defined as the natural capability to conceive and bear offspring. This ability is governed by a complex interplay of hormones, anatomy, and timing. For both males and females, fertility is not just about having the right parts; it’s about how these parts work together in harmony. Hormonal regulation plays a pivotal role, orchestrating everything from the menstrual cycle in females to sperm production in males. Understanding these biological mechanisms is essential to grasp how life begins and the challenges some may face in achieving conception.
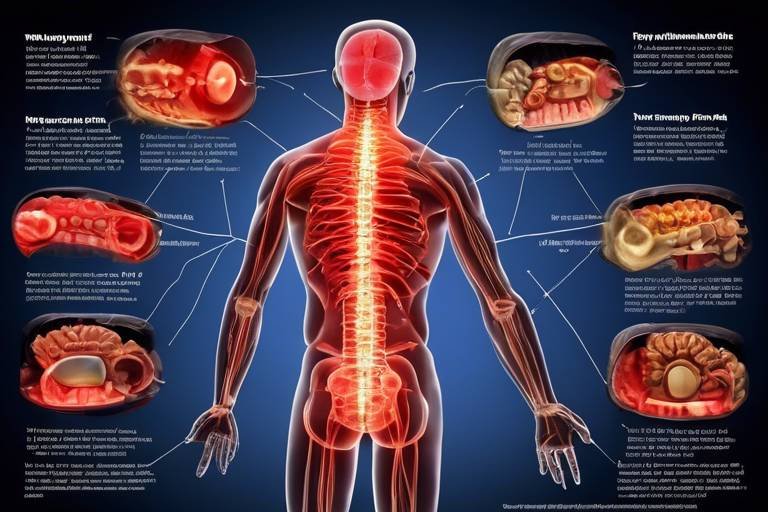
Before we delve into the specifics of fertility, it's essential to have a basic understanding of the reproductive anatomy in both males and females. The male and female reproductive systems are designed to work in concert to facilitate reproduction. Each system has its unique structures and functions that contribute to the overall process of conception. Recognizing these components allows us to appreciate the intricacies involved in bringing a new life into the world.
The female reproductive system is a marvel of biological engineering, consisting of various organs that play crucial roles in ovulation, fertilization, and pregnancy. Key structures include the ovaries, fallopian tubes, uterus, and vagina. Each of these components has a specific function that contributes to the reproductive process. For instance, the ovaries not only produce eggs but also secrete hormones that regulate the menstrual cycle. Understanding these structures is vital for anyone interested in fertility and reproductive health.
The ovaries are the powerhouses of the female reproductive system, responsible for producing eggs and hormones. Each month, during the menstrual cycle, one of the ovaries releases an egg in a process known as ovulation. This event is crucial for fertility, as it creates the opportunity for sperm to fertilize the egg. The hormonal fluctuations that accompany ovulation can affect mood, energy levels, and overall health. It's fascinating to think about how a single egg can lead to the creation of a new human being!
Once fertilization occurs, the journey continues into the uterus, which provides a nurturing environment for the developing embryo. The uterine lining, known as the endometrium, thickens in preparation for implantation. A healthy uterine environment is essential for a successful pregnancy. If the lining is not conducive to implantation, even a perfectly fertilized egg may struggle to develop. This highlights the importance of not only the egg and sperm but also the environment in which they meet and grow.
On the flip side, the male reproductive system is equally vital for reproduction. It is designed for the production and delivery of sperm. Key components include the testes, vas deferens, prostate, and seminal vesicles. The testes produce sperm and hormones like testosterone, which are crucial for male fertility. The vas deferens transports sperm during ejaculation, while the prostate and seminal vesicles contribute fluids that nourish and protect sperm. Understanding how these systems work together is essential for appreciating male fertility.
Several factors can influence fertility, making it a complex issue for many couples. Age, lifestyle choices, and underlying health conditions all play significant roles. For instance, as people age, their fertility tends to decline. This is particularly notable in women, where age can greatly affect both egg quality and quantity. Lifestyle choices, such as diet and exercise, can also impact reproductive health. Making informed choices can enhance fertility and improve overall well-being.
Age is one of the most significant factors affecting fertility for both men and women. As women age, particularly after their mid-30s, the quality and quantity of their eggs begin to decline. For men, while fertility may not decline as sharply, sperm quality can also decrease with age. This can have profound implications for family planning. Understanding the biological clock is essential for anyone considering starting a family.
Your lifestyle choices can have a substantial impact on your reproductive health. Factors such as diet, exercise, and substance use can either enhance or hinder fertility. For example, a balanced diet rich in vitamins and minerals can improve egg and sperm quality. On the other hand, smoking and excessive alcohol consumption can negatively affect fertility. Making healthy lifestyle choices is not just about improving fertility; it’s about enhancing overall health and well-being.
- What is the average age for women to conceive? Most women are most fertile in their 20s and early 30s.
- Can stress affect fertility? Yes, high stress levels can impact hormonal balance and fertility.
- How can I improve my fertility? Maintaining a healthy lifestyle, managing stress, and consulting with a healthcare provider can help.
- What role does diet play in fertility? A nutritious diet can enhance reproductive health and improve fertility outcomes.

Understanding Fertility
Fertility is an awe-inspiring biological phenomenon that refers to the natural capability of an individual to conceive and bear offspring. It's not just a simple process; it's a complex dance of hormones, cells, and organs working in harmony. When we dive into the world of fertility, we uncover a myriad of factors that influence our ability to create life. Have you ever wondered what really happens in our bodies when we try to conceive? Well, let's break it down!
At the heart of fertility are two key players: the male and female reproductive systems. Each system has its own unique anatomy and functions that contribute to the miracle of conception. In females, the ovaries release eggs during the menstrual cycle, while in males, the testes produce sperm. But it’s not just about the organs; the hormonal regulation that governs these processes is equally important. Hormones like estrogen and testosterone play pivotal roles, acting as the conductors in this biological orchestra.
To understand fertility better, we must also consider the timing of ovulation. Did you know that a woman is most fertile during a specific window each month? This is when an egg is released from the ovary and is available for fertilization. The menstrual cycle, which averages about 28 days, is a key factor in determining this fertile window. If you’re looking to conceive, tracking ovulation can be a game-changer!
Moreover, the environment in which conception occurs is crucial. The female reproductive tract is designed to support sperm survival and transport, while the uterus prepares itself to nurture a developing embryo. The intricate lining of the uterus, known as the endometrium, thickens in anticipation of a fertilized egg, creating a cozy space for implantation. If the conditions are right, and everything aligns perfectly, a new life can begin.
But wait, there’s more! Fertility isn't just about biology; it’s also influenced by a plethora of external factors. Age, for instance, plays a significant role in fertility for both men and women. As we age, our reproductive capabilities decline, which can impact family planning decisions. It's a stark reminder that time is a crucial factor in the journey of parenthood.
In addition to age, lifestyle choices can either enhance or hinder fertility. Diet, exercise, and even stress levels can have profound effects on reproductive health. For example, maintaining a balanced diet rich in vitamins and minerals can boost fertility, while excessive alcohol or drug use can decrease it. It's fascinating how our everyday choices can influence such a monumental aspect of our lives!
In summary, understanding fertility is about appreciating the complex interplay of biological processes, hormonal regulation, and external influences. By being aware of these factors, individuals can make informed decisions about their reproductive health, paving the way for a successful conception journey.
- What is the average age for women to conceive? Most women are most fertile in their 20s to early 30s. Fertility begins to decline after age 35.
- Can lifestyle changes improve fertility? Absolutely! A healthy diet, regular exercise, and avoiding harmful substances can enhance reproductive health.
- How can I track my ovulation? You can track ovulation through methods like calendar tracking, ovulation predictor kits, or monitoring physical signs like basal body temperature.
Reproductive Anatomy
Understanding the intricacies of reproductive anatomy is essential for grasping how fertility works. The male and female reproductive systems are complex networks of organs and glands that work together to ensure the continuation of species. Each component plays a vital role, from the production of gametes to the environment where fertilization and development occur. In this section, we will dive into the key structures involved in reproduction, their functions, and how they contribute to the miracle of life.
The female reproductive system is a remarkable assembly of organs designed for the production of eggs, the site of fertilization, and the nurturing of a developing fetus. It includes:
- Ovaries: These almond-shaped organs are responsible for producing eggs and hormones like estrogen and progesterone.
- Fallopian Tubes: These tubes transport the eggs from the ovaries to the uterus and are the typical site for fertilization.
- Uterus: A muscular organ where a fertilized egg implants and grows into a fetus.
- Vagina: This canal connects the external genitals to the uterus and serves as the birth canal during delivery.
Each of these components plays a critical role in the reproductive process. For instance, the ovaries not only produce eggs but also release hormones that regulate the menstrual cycle, influencing ovulation and fertility.
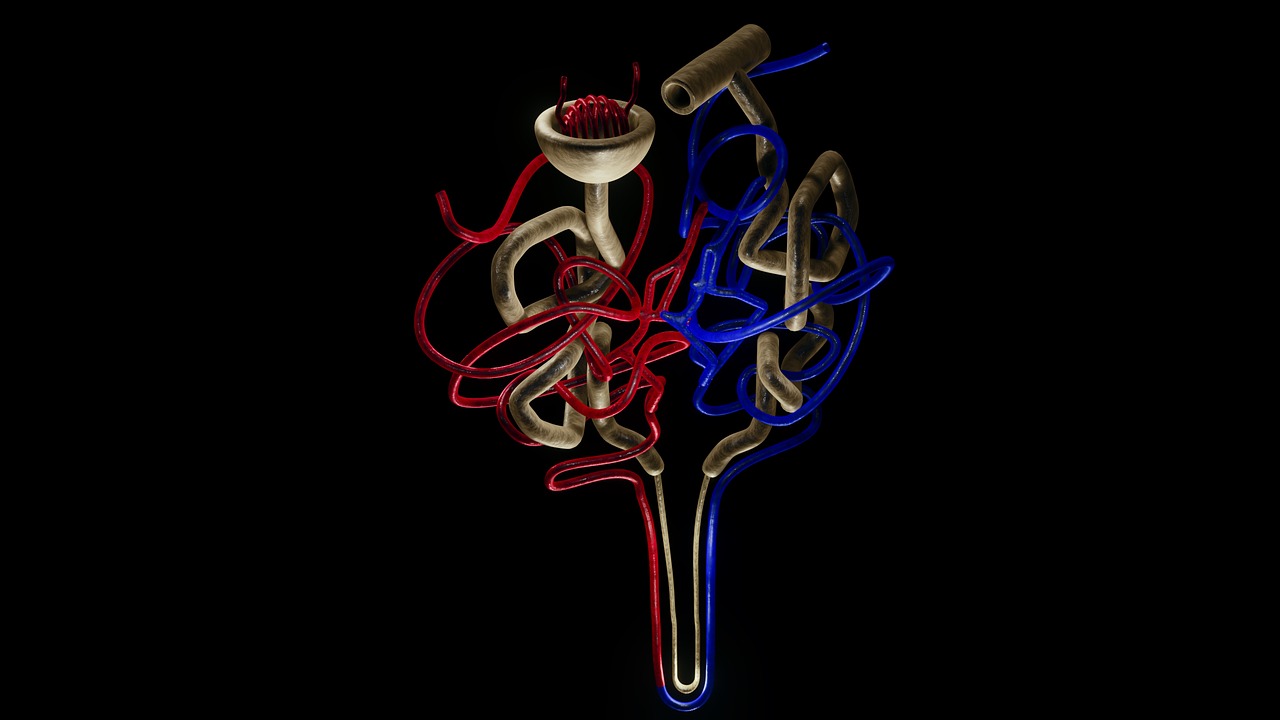
The ovaries are the powerhouse of the female reproductive system. They contain thousands of immature eggs, or follicles, and each month, during the menstrual cycle, one follicle matures and releases an egg in a process known as ovulation. This event is tightly regulated by hormones like luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Understanding how ovulation works is crucial for women trying to conceive, as it marks the optimal time for fertilization.
The uterus is often referred to as the womb, and it plays an essential role in supporting a developing embryo. The inner lining of the uterus, known as the endometrium, thickens in preparation for a fertilized egg. If implantation occurs, the endometrium provides the necessary nutrients and environment for the embryo to grow. However, if no fertilization takes place, the endometrium sheds during menstruation. The health of the uterine lining is vital; conditions like endometriosis or fibroids can significantly impact fertility.
Switching gears to the male reproductive system, this system is primarily focused on the production and delivery of sperm. It consists of:
- Testes: These are the male gonads responsible for producing sperm and testosterone.
- Vas Deferens: A muscular tube that transports sperm from the testes to the urethra.
- Prostate Gland: This gland produces a fluid that nourishes and helps transport sperm.
- Seminal Vesicles: These glands produce a sugary fluid that provides energy for the sperm and makes up a significant portion of semen.
The male reproductive system is a finely tuned mechanism where the testes produce millions of sperm daily. The journey of sperm from the testes through the vas deferens to the urethra is crucial for successful reproduction. Any disruption in this process can affect fertility.
In conclusion, the anatomy of the reproductive systems in both males and females is complex yet beautifully orchestrated. Understanding these structures and their functions not only enhances our knowledge of fertility but also empowers individuals with the information needed to make informed choices about reproductive health.
Q1: What is the primary function of the ovaries?
A1: The primary function of the ovaries is to produce eggs and hormones that regulate the menstrual cycle and overall reproductive health.
Q2: How does age affect fertility in women?
A2: Fertility in women typically declines with age, particularly after the age of 35, due to a decrease in the quantity and quality of eggs.
Q3: What role does the prostate gland play in reproduction?
A3: The prostate gland produces a fluid that nourishes and helps transport sperm, playing a critical role in male fertility.

Female Reproductive System
The is a complex and fascinating network of organs that work in harmony to achieve one of nature's most remarkable processes: reproduction. At the core of this system are the ovaries, fallopian tubes, uterus, and vagina, each playing a vital role in the journey from ovulation to childbirth. Understanding these components is crucial for grasping how fertility operates and the factors that can influence it.
Let’s start with the ovaries. These small, almond-shaped organs are not just responsible for producing eggs; they also secrete hormones like estrogen and progesterone, which are essential for regulating the menstrual cycle and preparing the body for potential pregnancy. Each month, during a process known as the menstrual cycle, one ovary releases an egg in a phase called ovulation. This is a critical moment in the fertility timeline, as the egg then travels down the fallopian tube, where it may meet sperm for fertilization.
Next up, we have the fallopian tubes. These slender tubes are the pathways through which the egg travels after ovulation. If sperm is present, fertilization usually occurs here. It’s fascinating to think about how these tubes act as the bridge between the ovaries and the uterus, creating a connection that is essential for conception. If the fertilized egg successfully navigates this journey, it will implant itself into the uterus.
The uterus is often referred to as the "womb" and is a critical player in the reproductive process. Its primary function is to provide a nurturing environment for a developing embryo. The inner lining of the uterus, known as the endometrium, thickens each month in preparation for a potential pregnancy. If implantation occurs, the uterus supports the embryo as it grows, providing nourishment and protection. However, if fertilization does not occur, the body sheds this lining during menstruation, and the cycle begins anew.
Finally, the vagina serves as the birth canal and the passage through which sperm enters the female body. It plays a crucial role during intercourse and childbirth, adapting to accommodate the needs of each process. The vaginal walls are elastic and can stretch significantly, allowing for the safe delivery of a baby, while also providing a suitable environment for the sperm to travel toward the uterus.
Understanding the female reproductive system is not just about knowing the anatomy; it’s about appreciating how these organs work together in a delicate balance. Factors such as hormonal fluctuations, age, and overall health can influence this system, making it essential for women to monitor their reproductive health closely. Awareness of how each component functions can empower women to make informed decisions about their fertility and reproductive choices.
- What is the primary function of the ovaries? The ovaries produce eggs and hormones that regulate the menstrual cycle.
- How does the menstrual cycle affect fertility? The menstrual cycle prepares the body for potential pregnancy, with ovulation marking the time when conception is most likely.
- What role does the uterus play in pregnancy? The uterus provides a nurturing environment for a fertilized egg to implant and develop into a fetus.
- Why is it important to understand the female reproductive system? Understanding this system helps women make informed decisions about their reproductive health and fertility.

Ovaries and Ovulation
The ovaries are two small, almond-shaped organs located on either side of the uterus, and they play a pivotal role in the female reproductive system. Each ovary is responsible for producing and releasing eggs, as well as secreting hormones such as estrogen and progesterone. These hormones are crucial for regulating the menstrual cycle and maintaining reproductive health. The process of ovulation is a key aspect of fertility, as it marks the time when an egg is released from the ovary, making it available for fertilization.
Understanding the menstrual cycle is essential to grasp how ovulation works. Typically, a menstrual cycle lasts about 28 days, but it can vary from person to person. The cycle can be divided into several phases:
- Follicular Phase: This phase begins on the first day of menstruation and lasts until ovulation. During this time, the follicles in the ovaries mature, and one follicle becomes dominant, preparing to release an egg.
- Ovulation: Around the midpoint of the cycle, usually between days 12 and 16, a surge in luteinizing hormone (LH) triggers the release of the mature egg from the dominant follicle. This is the prime time for conception.
- Luteal Phase: After ovulation, the ruptured follicle transforms into the corpus luteum, which produces progesterone to prepare the uterine lining for potential implantation of a fertilized egg.
During ovulation, the egg travels down the fallopian tube, where it may encounter sperm. If fertilization occurs, the fertilized egg will implant itself in the uterine lining, leading to pregnancy. If not, the egg will disintegrate, and the cycle will begin anew with menstruation.
It's fascinating to note that a woman is born with all the eggs she will ever have—approximately one to two million. However, by the time she reaches puberty, this number dwindles to around 300,000 to 400,000. Each month, during the menstrual cycle, several follicles start to develop, but typically only one egg will be ovulated. The rest will undergo a process called atresia, which is the degeneration of ovarian follicles that do not mature. This natural selection process ensures that only the healthiest egg is released during ovulation.
Understanding the health of the ovaries and the process of ovulation is vital for women who are trying to conceive. Factors such as hormonal imbalances, stress, and lifestyle choices can significantly impact ovulation and overall fertility. Therefore, maintaining a healthy lifestyle, managing stress, and consulting healthcare providers for regular check-ups can enhance reproductive health and increase the chances of conception.
- What is ovulation? Ovulation is the process in which a mature egg is released from the ovary, typically occurring around the midpoint of the menstrual cycle.
- How can I track my ovulation? You can track ovulation using methods such as calendar tracking, ovulation predictor kits, or monitoring changes in basal body temperature.
- What factors can affect ovulation? Factors such as stress, hormonal imbalances, age, and lifestyle choices like diet and exercise can all impact ovulation.

Uterine Environment
The plays a pivotal role in the journey of conception and the nurturing of a developing embryo. Think of the uterus as a cozy, welcoming home where a new life can grow and thrive. This organ is not just a passive structure; it actively prepares itself each month to provide the perfect conditions for implantation and pregnancy. The health of the uterine lining, known as the endometrium, is crucial in this process. If the endometrium is thick, well-vascularized, and hormonally balanced, it creates an ideal setting for the fertilized egg to latch on and begin its miraculous development.
During the menstrual cycle, the uterus undergoes various changes influenced by hormones such as estrogen and progesterone. In the first half of the cycle, estrogen levels rise, leading to the thickening of the endometrium. This phase is essential because it prepares the uterus for a potential pregnancy. If fertilization does not occur, hormone levels drop, leading to the shedding of the uterine lining during menstruation. However, when conception does happen, the embryo releases hormones that signal the uterus to maintain its lining, thereby preventing menstruation and allowing for the embryo to embed itself securely.
Moreover, the health of the uterine environment can be affected by several factors. Here are some key points to consider:
- Hormonal Balance: Imbalances in hormones can lead to issues like endometriosis or uterine fibroids, which can hinder implantation and overall reproductive health.
- Nutritional Factors: A diet rich in vitamins and minerals is essential for maintaining a healthy uterine lining. Nutrients like folic acid, vitamin D, and omega-3 fatty acids play significant roles in reproductive health.
- Age: As women age, the quality of the uterine lining can decline, impacting fertility and the ability to sustain a pregnancy.
In summary, the uterine environment is not merely a backdrop for pregnancy; it is an active participant in the reproductive process. Ensuring that this environment is healthy and conducive to implantation is key for women who are trying to conceive. Regular check-ups with a healthcare provider can help identify any underlying issues that might affect uterine health, allowing for timely interventions and better outcomes in the journey to parenthood.
Q: What can I do to improve my uterine environment?
A: Maintaining a balanced diet, managing stress, and regular exercise can significantly enhance uterine health. Additionally, consulting with a healthcare provider for personalized advice is beneficial.
Q: How does age affect the uterine environment?
A: As women age, hormonal changes can affect the thickness and health of the uterine lining, which may impact fertility and the ability to carry a pregnancy to term.
Q: Are there any medical conditions that affect the uterine environment?
A: Yes, conditions like endometriosis, fibroids, and polyps can negatively impact the uterine lining and overall fertility. Regular screenings can help detect these issues early.

Male Reproductive System
The male reproductive system is a fascinating and intricate network of organs and structures designed for the production and delivery of sperm. At its core, this system plays a crucial role in human reproduction, ensuring that the male gametes are not only produced but also transported effectively to meet the female gametes. Understanding the anatomy of the male reproductive system can shed light on how fertility works and what factors can influence it.
Key components of the male reproductive system include:
- Testes: These are the primary reproductive organs responsible for producing sperm and hormones, particularly testosterone. The testes are located in the scrotum, which helps regulate their temperature, essential for optimal sperm production.
- Epididymis: After sperm are produced in the testes, they move to the epididymis, a coiled tube where they mature and are stored until ejaculation.
- Vas Deferens: This muscular tube transports mature sperm from the epididymis to the ejaculatory duct. It plays a vital role in the journey of sperm as they prepare for potential fertilization.
- Seminal Vesicles: These glands produce a significant portion of the seminal fluid, which nourishes and helps transport sperm during ejaculation.
- Prostate Gland: This gland adds additional fluid to the semen, enhancing sperm motility and viability. It also plays a role in the overall health of the male reproductive system.
- Urethra: This dual-purpose tube carries urine from the bladder and semen from the reproductive tract out of the body. It is the final pathway for sperm during ejaculation.
Each of these components works in harmony to ensure that sperm production and delivery are efficient. The testes, for instance, are not just about sperm production; they also produce hormones that regulate various bodily functions, including libido and muscle mass. The journey of sperm is quite remarkable, starting from the testes, maturing in the epididymis, and then traveling through the vas deferens, where they mix with seminal fluid to form semen.
Moreover, the prostate gland and seminal vesicles significantly impact the quality of the semen. The fluid they produce is rich in nutrients and enzymes that help maintain the viability of sperm, ensuring they can survive the journey through the female reproductive tract. This is crucial, as only a small percentage of sperm will ultimately reach the egg for fertilization.
Understanding the male reproductive system is essential not only for comprehending how conception occurs but also for recognizing the various factors that can affect male fertility. Issues such as hormonal imbalances, structural abnormalities, and lifestyle choices can all play a role in a man's reproductive health.
Q: How does age affect male fertility?
A: While males can remain fertile into older age, sperm quality and quantity can decline over time, making it more challenging to conceive.
Q: What lifestyle changes can improve male fertility?
A: Maintaining a healthy diet, exercising regularly, avoiding smoking and excessive alcohol, and managing stress can significantly enhance fertility.
Q: Can medical conditions impact male fertility?
A: Yes, conditions such as diabetes, hormonal disorders, and certain infections can adversely affect sperm production and overall reproductive health.

Factors Affecting Fertility
When it comes to fertility, it's not just about the biological clock ticking away; there are a myriad of factors that can either boost or hinder your chances of conception. Understanding these factors is crucial for anyone looking to start or expand their family. It's like trying to bake a cake—if you miss a key ingredient, the whole thing can fall flat! In this section, we’ll dive into the various elements that can impact reproductive health and the likelihood of conception.
One of the most significant factors affecting fertility is age. As we age, our bodies undergo natural changes that can affect our reproductive capabilities. For women, the quantity and quality of eggs decline with age, particularly after the age of 35. Men also experience a gradual decline in sperm quality and quantity as they get older. This means that if you’re planning to have kids, timing can be everything. It’s crucial to have open conversations about family planning and consider how age might play a role in your journey.
Another major player in the fertility game is lifestyle choices. What we eat, how much we move, and even our social habits can either enhance or diminish our reproductive health. For instance, a diet rich in fruits, vegetables, whole grains, and healthy fats can provide essential nutrients that support fertility. On the flip side, excessive alcohol consumption, smoking, and drug use can wreak havoc on reproductive systems. Here’s a quick look at how different lifestyle choices can impact fertility:
| Lifestyle Choice | Impact on Fertility |
|---|---|
| Balanced Diet | Enhances overall health and fertility |
| Regular Exercise | Improves hormonal balance and reduces stress |
| Smoking | Decreases sperm quality and egg health |
| Alcohol Consumption | Can lead to hormonal imbalances and reduced fertility |
Additionally, underlying health conditions can significantly impact fertility. Conditions such as polycystic ovary syndrome (PCOS), endometriosis, and thyroid disorders can create hurdles on the path to conception. It's essential to consult healthcare professionals who can provide guidance and treatment options. Think of your body as a finely tuned machine; if one part isn’t working well, it can affect the entire system.
Stress is another factor that many people overlook. When life gets overwhelming, the body can react in ways that affect fertility. High stress levels can lead to hormonal imbalances, which in turn can disrupt ovulation and sperm production. Finding ways to manage stress—be it through yoga, meditation, or simply taking time for self-care—can be beneficial not just for your mental health but also for your reproductive health.
Lastly, environmental factors should not be ignored. Exposure to certain chemicals and pollutants can negatively impact fertility. For instance, heavy metals, pesticides, and even some plastics have been linked to reproductive issues. It’s wise to be mindful of the products you use and the environments you frequent. Sometimes, making small changes in your surroundings can lead to significant improvements in your fertility health.
In summary, understanding the factors that affect fertility is not just about knowing what can go wrong; it’s also about empowering yourself to make informed decisions. Whether it’s paying attention to your age, making healthier lifestyle choices, managing stress, or being aware of environmental impacts, every little bit helps. Remember, the journey to conception is often a marathon, not a sprint!
- What age is considered too late to conceive? While women can technically conceive until menopause, fertility significantly declines after age 35. For men, while there’s no definitive age limit, sperm quality tends to decrease with age.
- How can I improve my fertility? Focus on a balanced diet, regular exercise, managing stress, and avoiding harmful substances like tobacco and excessive alcohol.
- Can stress really affect my fertility? Yes, high stress levels can disrupt hormonal balance, which can impact ovulation and sperm production.
- Are there specific health conditions that affect fertility? Yes, conditions like PCOS, endometriosis, and thyroid disorders can create challenges in conceiving.

Age and Fertility
When it comes to fertility, age is a significant factor that cannot be overlooked. As we journey through life, our bodies undergo various changes, and these changes can have profound effects on our reproductive capabilities. For women, fertility tends to peak in their late teens to early twenties, gradually declining as they approach their thirties and forties. This decline is often attributed to a decrease in both the quantity and quality of eggs produced. Did you know that by age 35, a woman’s chances of conceiving naturally start to drop significantly? This is a stark reminder of how time influences our biological clock.
On the other hand, men also experience a decline in fertility as they age, although the changes are often more gradual. Sperm production may decrease, and the quality of sperm can diminish, leading to lower fertility rates. The age-related decline in male fertility can result in issues such as decreased sperm motility and increased chances of genetic abnormalities in sperm. This is crucial to consider, especially for couples trying to conceive later in life.
To illustrate how age impacts fertility, let’s take a look at some statistics:
| Age Range | Female Fertility Rate | Male Fertility Rate |
|---|---|---|
| 20-24 | 85% chance of conception | Peak fertility |
| 25-29 | 75% chance of conception | High fertility |
| 30-34 | 60% chance of conception | Gradual decline |
| 35-39 | 50% chance of conception | Notable decline |
| 40+ | 20% chance of conception | Significant decline |
These figures highlight the stark reality that age plays a crucial role in fertility. For many couples, understanding this biological timeline can help in making informed decisions about family planning. It’s essential to have open conversations about reproductive health, especially as one approaches the age milestones that could impact fertility.
In addition to biological factors, societal and personal circumstances often dictate when individuals or couples decide to start a family. With the rise of career-focused lifestyles and advancements in reproductive technology, many are choosing to delay parenthood. While this can be a fulfilling choice, it’s vital to remain aware of the potential challenges that may arise due to aging. Consulting with healthcare professionals can provide valuable insights and guidance tailored to individual circumstances.
In conclusion, age is an undeniable factor in fertility for both men and women. As we navigate through life, being proactive about our reproductive health can lead to better outcomes. Whether you’re considering starting a family now or in the future, understanding the implications of age on fertility is key to making informed decisions.
- What age is considered the best for women to conceive? Generally, the late teens to early twenties is considered the peak fertility age for women.
- Can men experience infertility as they age? Yes, men can also experience a decline in fertility as they age, although it tends to be more gradual.
- Are there ways to improve fertility as I age? Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding harmful substances can help improve fertility.

Lifestyle Choices
When it comes to fertility, the choices we make in our daily lives can have a profound impact. It's almost like nurturing a garden; if you want your plants to thrive, you need to give them the right conditions. Similarly, our bodies require a healthy environment to optimize reproductive health. Let’s dive into some key lifestyle choices that can either enhance or hinder our chances of conception.
First up, let’s talk about nutrition. Eating a balanced diet rich in vitamins and minerals is crucial for both men and women. Foods that are high in antioxidants, such as fruits and vegetables, can help reduce oxidative stress, which is known to affect fertility. For instance, incorporating foods like berries, nuts, and leafy greens can be beneficial. On the flip side, diets high in processed foods and sugars can lead to weight gain and hormonal imbalances, both of which may negatively impact fertility.
Next, we can't overlook the importance of exercise. Regular physical activity is not just about fitting into your favorite jeans; it plays a vital role in regulating hormones and maintaining a healthy weight. However, moderation is key. While a good workout can boost your fertility, excessive exercise can lead to a decrease in ovulation for women and lower sperm counts for men. Striking a balance is essential. Think of it as tuning a musical instrument; too much tension can throw everything off.
Another major factor is substance use. Smoking, excessive alcohol consumption, and recreational drugs can wreak havoc on reproductive health. Studies have shown that smoking can lead to reduced fertility in both genders, while heavy drinking can disrupt hormonal balance and ovulation. If you’re serious about starting a family, it might be time to reassess these habits. You wouldn’t want to build a house on a shaky foundation, right?
Moreover, managing stress levels is crucial. Stress can be a silent saboteur of fertility. When we’re stressed, our bodies produce cortisol, which can interfere with the hormones responsible for ovulation and sperm production. Finding ways to relax, whether through yoga, meditation, or simply enjoying a good book, can create a more favorable environment for conception. Think of stress as a fog; it can cloud your vision and make it hard to see the path ahead.
Lastly, it’s important to consider medical factors. Regular check-ups with healthcare providers can help identify any underlying health issues that may affect fertility. Conditions such as polycystic ovary syndrome (PCOS) or thyroid disorders can be managed effectively with medical guidance. Just like a car needs regular maintenance to run smoothly, our bodies require the same level of care and attention.
In summary, making informed lifestyle choices can significantly influence fertility. By focusing on nutrition, exercise, substance use, stress management, and regular medical check-ups, you can create a nurturing environment for conception. Remember, every small change can lead to big results in the journey toward parenthood.
- Can diet really affect fertility? Yes, a balanced diet rich in essential nutrients can improve reproductive health.
- Is exercise beneficial for fertility? Moderate exercise can help regulate hormones, but excessive exercise may have the opposite effect.
- How does stress influence fertility? High stress levels can disrupt hormonal balance, affecting ovulation and sperm production.
- What lifestyle changes should I consider for better fertility? Focus on a healthy diet, regular moderate exercise, avoiding harmful substances, and managing stress.
Frequently Asked Questions
- What is fertility?
Fertility refers to the natural ability to conceive and bear children. It encompasses the biological processes that enable reproduction in both males and females, including hormonal regulation and reproductive anatomy.
- How does the female reproductive system work?
The female reproductive system includes several key organs such as the ovaries, fallopian tubes, uterus, and vagina. The ovaries produce eggs and hormones, while the uterus provides a nurturing environment for a developing embryo. Understanding how these organs function is essential for grasping the complexities of fertility.
- What role do ovaries play in fertility?
Ovaries are crucial for fertility as they produce eggs and hormones that regulate the menstrual cycle. The process of ovulation, where an egg is released, is vital for conception. Any disruption in this process can impact a woman's ability to conceive.
- How does age affect fertility?
Age significantly influences fertility for both men and women. As individuals age, the quality and quantity of eggs in women decline, while men may experience reduced sperm quality. This decline can affect family planning decisions and the likelihood of conception.
- What lifestyle choices can enhance fertility?
Healthy lifestyle choices play a crucial role in enhancing fertility. Factors like maintaining a balanced diet, engaging in regular exercise, avoiding smoking, and limiting alcohol consumption can positively impact reproductive health and increase the chances of conception.
- How does the uterine environment affect pregnancy?
The uterine environment is vital for successful implantation and pregnancy. A healthy uterine lining supports embryo development, while abnormalities can lead to complications. Ensuring uterine health is essential for those trying to conceive.
- What are common factors that affect fertility?
Several factors can influence fertility, including age, lifestyle choices, medical conditions, and environmental factors. Understanding these elements can help individuals make informed decisions about their reproductive health.