The Biology of Blood Types - What You Should Know
Welcome to the fascinating world of blood types, where biology meets medicine in an intricate dance of compatibility and health. Understanding blood types is not just a matter of trivia; it’s a vital aspect of medical science that can mean the difference between life and death in critical situations. From blood transfusions to organ transplants, the significance of knowing your blood type cannot be overstated. But what exactly are blood types, and why do they matter so much? Let’s dive into the biological significance, inheritance patterns, and implications for health and medicine.
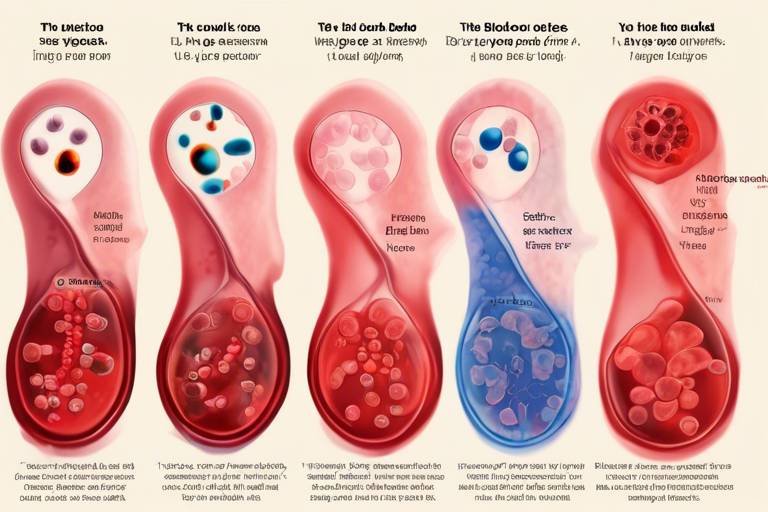
At the core of blood typing lies the concept of antigens and antibodies. Blood types are classified based on the presence of specific antigens on the surface of red blood cells. The most widely recognized systems are the ABO and Rh systems, which dictate compatibility for transfusions and organ transplants. Each blood type can trigger different immune responses, making it crucial to match donors and recipients correctly. Imagine blood types as a unique key that only fits into its corresponding lock; mismatched types can lead to severe complications.
The ABO blood group system categorizes blood into four main types: A, B, AB, and O. Each type has its own unique antigenic properties that influence immune responses and transfusion compatibility. For example, Type A blood has A antigens, while Type B has B antigens. Type AB blood has both, and Type O has neither, making it a universal donor. Understanding these differences is essential for safe medical practices.
Type A blood contains A antigens on the surface of red blood cells and anti-B antibodies in the plasma. This blood type is prevalent across various populations, with a significant portion of the world’s population being Type A. The compatibility of Type A blood with other types is crucial for safe blood transfusions. For instance, Type A individuals can receive blood from Type A and Type O donors, but they cannot receive Type B or AB blood without risking a serious immune reaction.
Type A blood is one of the most common blood types worldwide. Its distribution varies by population and geography, influencing transfusion practices and organ donation strategies. For example, in some regions, Type A may be more prevalent than Type O, which is often considered the universal donor type. Understanding these demographics can help healthcare providers make informed decisions about blood donations and transfusions.
Understanding the compatibility of Type A blood with other types is vital for safe blood transfusions. Type A individuals can receive:
- Type A blood
- Type O blood (universal donor)
However, they should avoid Type B and AB blood to prevent severe transfusion reactions. Such knowledge is critical for healthcare providers and patients alike.
Type B blood is characterized by B antigens and anti-A antibodies. This type is less common than Type A but still plays a significant role in blood donation and transfusion practices. Like Type A, Type B individuals must be cautious about compatibility; they can receive blood from Type B and Type O donors but should avoid Type A and AB blood.
The Rh factor adds another layer of complexity to blood typing. It determines whether blood is positive or negative. For instance, someone with Type A blood can be either A+ (Rh positive) or A- (Rh negative). This distinction is crucial, especially during pregnancy and blood transfusions, as Rh incompatibility can lead to serious health issues.
The distinction between Rh positive and Rh negative blood types plays a crucial role in medical procedures. Rh positive individuals can receive blood from both Rh positive and negative donors, while Rh negative individuals should only receive Rh negative blood. This knowledge is essential for patient safety and effective treatment.
The Rh factor has significant implications during pregnancy, particularly in cases of Rh incompatibility. If an Rh-negative mother is carrying an Rh-positive baby, her body may produce antibodies against the baby's blood cells, leading to complications. Monitoring Rh status in expectant mothers is vital to prevent potential health risks for both mother and child.
Blood types are inherited from parents based on genetic combinations. Understanding the genetics behind blood type inheritance can help predict a child's blood type. For instance, if both parents have Type A blood, their offspring could be Type A or Type O, depending on the genetic alleles inherited.
Genotypes play a crucial role in determining an individual's blood type. The combinations of alleles from parents can lead to various blood types observed in the population. For example, a child of one Type A parent and one Type B parent could inherit Type A, B, AB, or O blood, depending on the alleles received.
By understanding the inheritance patterns of blood types, parents can predict the possible blood types of their children. This knowledge can help in planning for medical needs and understanding family health histories.
Blood typing is essential in various medical settings, including surgeries, transfusions, and organ transplants. Accurate blood typing is critical for patient care and can significantly impact treatment outcomes. For instance, mismatched blood transfusions can lead to severe complications, including shock and organ failure.
Ensuring safe blood transfusions is vital for patient health. Protocols and testing methods are in place to confirm blood type compatibility before transfusions. These include cross-matching tests, which help identify potential reactions between donor and recipient blood.
In organ transplantation, blood type compatibility is crucial for successful outcomes. Donor-recipient matching based on blood types can significantly influence transplant success rates. For example, a mismatch can lead to organ rejection, making it essential for healthcare providers to consider blood types in their evaluations.
Emerging research continues to explore the complexities of blood types, including their roles in disease susceptibility and treatment responses. Understanding these relationships can open new avenues for personalized medicine and targeted therapies.
Studies suggest that certain blood types may be linked to varying susceptibility to diseases. For example, some research indicates that individuals with Type O blood may have a lower risk of certain infections. This section reviews current research findings and implications for public health.
Technological advancements are enhancing blood typing accuracy and efficiency. New methods and tools are improving blood typing processes in medical settings, ensuring that patients receive the safest and most effective care possible.
Q: Why is it important to know your blood type?
A: Knowing your blood type is crucial for safe blood transfusions, organ donations, and understanding potential health risks.
Q: Can blood types change over time?
A: Generally, blood types remain the same throughout a person's life unless there is a rare occurrence of a blood type change due to specific medical conditions.
Q: How can I find out my blood type?
A: You can find out your blood type through a simple blood test at a medical facility or by using at-home blood typing kits.

The Basics of Blood Types
Blood types are not just a trivial detail; they are a fundamental aspect of human biology that plays a critical role in medicine and health. At the core of blood typing are specific antigens found on the surface of red blood cells. These antigens are like tiny flags that signal to the immune system whether the blood is recognized as "self" or "foreign." The most widely recognized systems for classifying blood types are the ABO system and the Rh factor.
The ABO system is particularly interesting because it categorizes blood into four main types: A, B, AB, and O. Each type has its own unique set of antigens and antibodies, influencing not only transfusion compatibility but also how our bodies respond to infections and diseases. Understanding these blood types goes beyond just knowing your own; it can save lives in critical situations.
For instance, in emergency medical situations, knowing a patient's blood type can be the difference between life and death. If someone with Type A blood receives Type B blood, their immune system may react violently, leading to severe complications. This is why blood typing is essential for safe transfusions and organ transplants. With that said, let’s dive deeper into the two main systems of blood classification.
| Blood Type | Antigens Present | Antibodies Present | Compatibility |
|---|---|---|---|
| A | A antigens | Anti-B antibodies | A, O |
| B | B antigens | Anti-A antibodies | B, O |
| AB | A and B antigens | None | A, B, AB, O (Universal Recipient) |
| O | No antigens | Anti-A and Anti-B antibodies | O (Universal Donor) |
In addition to the ABO system, we also have the Rh factor, which determines whether your blood is positive or negative. This factor is another layer of complexity that can significantly impact transfusion protocols and pregnancy. For example, if an Rh-negative mother carries an Rh-positive baby, there can be complications that require careful monitoring and intervention.
In summary, understanding blood types is not just a matter of trivia; it has real-world implications for health and safety. Whether it’s for blood transfusions, organ donations, or pregnancy management, the basics of blood types are crucial knowledge for anyone looking to navigate the fascinating world of human biology.

The ABO Blood Group System
The ABO blood group system is one of the most significant classifications of blood types, impacting everything from transfusions to organ transplants. This system categorizes blood into four primary types: A, B, AB, and O. Each blood type is defined by the presence or absence of specific antigens on the surface of red blood cells, which are crucial for determining compatibility between donors and recipients. Understanding these blood types is not just an academic exercise; it has real-world implications for medical procedures and patient safety.
To grasp the importance of the ABO blood group system, it's essential to recognize that each blood type has unique antigenic properties. For instance, individuals with Type A blood have A antigens on their red blood cells and produce anti-B antibodies in their plasma. Conversely, those with Type B blood possess B antigens and anti-A antibodies. Type AB blood is unique as it contains both A and B antigens, meaning individuals with this type can receive blood from any ABO group, making them universal recipients. On the other hand, individuals with Type O blood lack A and B antigens, but they have both anti-A and anti-B antibodies, which makes them universal donors.
The implications of these classifications extend beyond mere compatibility; they also influence immune responses. For example, if a person with Type A blood receives Type B blood, their immune system may recognize the B antigens as foreign and mount an attack, leading to serious complications. This highlights the necessity for accurate blood typing before any transfusion or transplantation procedure.
| Blood Type | Antigens Present | Antibodies Present | Compatible Blood Types |
|---|---|---|---|
| A | A | Anti-B | A, O |
| B | B | Anti-A | B, O |
| AB | A and B | None | A, B, AB, O |
| O | None | Anti-A and Anti-B | O |
In summary, the ABO blood group system is not just a biological curiosity; it is a critical component of modern medicine. Understanding the differences between these blood types can save lives by ensuring safe and effective transfusions and organ transplants. As we continue to advance in medical science, the importance of blood type compatibility will only grow, making it essential for both healthcare professionals and patients to be informed.

Type A Blood
Type A blood is an intriguing and vital component of the human blood classification system. It is characterized by the presence of A antigens on the surface of red blood cells, alongside anti-B antibodies in the plasma. This unique combination not only defines Type A blood but also influences how the immune system reacts to different blood types during transfusions and organ transplants. Understanding the properties of Type A blood can help us appreciate its role in medical settings and everyday life.
When it comes to prevalence, Type A blood is one of the most common blood types globally. Its distribution varies across different populations and geographical regions. For example, in Europe, Type A is quite prevalent, while in some Asian countries, it might be less common. This variation can significantly impact transfusion practices and organ donation strategies. Knowing the prevalence of Type A blood can help healthcare professionals make informed decisions when matching donors and recipients.
Compatibility is a critical aspect of Type A blood that deserves special attention. When it comes to blood transfusions, understanding which blood types can be safely transfused into Type A individuals is essential. Here’s a quick compatibility guide:
| Blood Type | Can Donate To Type A | Can Receive From Type A |
|---|---|---|
| Type A | Yes | Yes |
| Type O | Yes | Yes |
| Type B | No | No |
| Type AB | No | Yes |
As illustrated in the table, Type A individuals can receive blood from Type A and Type O donors, making Type O a universal donor for them. However, they cannot receive blood from Type B donors, as this could trigger an immune response due to the presence of anti-B antibodies. This compatibility knowledge is crucial for healthcare providers, ensuring that patients receive the safest possible transfusions.
In summary, Type A blood is not just another classification; it plays a significant role in the medical field and in individual health. Its unique properties, prevalence, and compatibility with other blood types are essential for safe medical practices. Understanding Type A blood can empower individuals to make informed decisions about their health and medical care.
- What is the most common blood type? Type O is generally considered the most common blood type worldwide, followed by Type A.
- Can Type A blood donate to Type AB? Yes, Type A blood can donate to Type AB individuals, as AB recipients can receive blood from all types.
- Is there a special diet for people with Type A blood? Some believe that individuals with Type A blood may benefit from a vegetarian diet, though scientific evidence is limited.
- How can I find out my blood type? You can determine your blood type through a blood test at a medical facility or by using at-home blood typing kits.

Prevalence of Type A Blood
Type A blood is one of the most common blood types globally, and its prevalence varies significantly across different populations and geographical regions. In fact, studies have shown that approximately 26% to 30% of the world's population has Type A blood. This percentage can fluctuate based on ethnic and regional backgrounds. For instance, Type A blood is more prevalent in European populations, where it can account for nearly 40% of the blood types. In contrast, in certain Asian populations, the prevalence can drop to 20% or lower.
Understanding the distribution of Type A blood is not just an academic exercise; it has practical implications for healthcare systems around the world. For example, in regions where Type A blood is more common, blood banks can stockpile this type more efficiently, ensuring that there is a sufficient supply for those in need. Conversely, in areas where Type A blood is less common, hospitals may face challenges in matching donors with recipients, which can complicate medical procedures.
Here’s a brief overview of Type A blood prevalence in different regions:
| Region | Prevalence of Type A Blood |
|---|---|
| North America | 30% |
| Europe | 40% |
| Asia | 20% |
| Africa | 25% |
As we delve deeper into the implications of this prevalence, it becomes clear that Type A blood's significance extends beyond mere statistics. Its commonality can influence everything from transfusion practices to organ donation strategies. For instance, hospitals in regions with a higher prevalence of Type A blood may find it easier to perform successful transfusions, as the likelihood of finding compatible donors increases.
Moreover, the cultural and societal factors that influence blood type distribution are equally fascinating. In some cultures, blood type is even believed to play a role in personality traits and compatibility in relationships, adding a layer of intrigue to the biological significance of blood types.
In conclusion, the prevalence of Type A blood is not just a number; it represents a critical aspect of our biological makeup that has far-reaching implications for healthcare and society at large. Understanding these patterns can help us better prepare for medical needs and foster a greater appreciation for the diversity of human biology.

Compatibility of Type A Blood
When it comes to blood transfusions, understanding the compatibility of Type A blood is crucial for ensuring the safety and health of patients. Type A blood has A antigens on the surface of its red blood cells and contains anti-B antibodies in the plasma. This unique combination plays a significant role in determining which blood types can be safely transfused into individuals with Type A blood.
For a successful transfusion, it is essential to match the donor's blood type with that of the recipient. Type A individuals can receive blood from several compatible sources:
- Type A - The most straightforward option, Type A blood can be transfused into Type A recipients without any issues.
- Type O - This universal donor type is compatible with all blood types, making it a safe choice for Type A individuals.
- Type AB - While not as common, Type AB blood can also be accepted by Type A recipients, but this is generally less favorable due to the presence of B antigens.
However, it is crucial to avoid transfusing Type B or Type AB blood into a Type A individual, as the anti-B antibodies present in Type A plasma will attack the B antigens, leading to potentially severe reactions. Understanding these compatibilities not only aids in safe transfusions but also helps in planning for surgeries and emergency medical situations.
In summary, the compatibility of Type A blood is relatively straightforward, allowing for transfusions from Type A and Type O donors. However, caution must be exercised to prevent complications from incompatible blood types. This knowledge is vital for healthcare providers and patients alike, ensuring that every blood transfusion is a step toward healing rather than a risk.
- What happens if Type A blood receives Type B blood?
Receiving Type B blood can lead to a severe immune reaction, as the anti-B antibodies in Type A blood will attack the B antigens, potentially causing life-threatening complications. - Can Type A blood donate to other blood types?
Type A blood can donate to Type A and AB recipients, making it a valuable type for those in need of transfusions. - Why is Type O considered the universal donor?
Type O blood lacks A and B antigens, allowing it to be transfused to any blood type without triggering an immune response.

Type B Blood
is an intriguing category within the ABO blood group system, characterized by the presence of B antigens on the surface of red blood cells and the corresponding anti-A antibodies in the plasma. This unique combination not only defines Type B blood but also plays a significant role in determining compatibility for blood transfusions and organ transplants. Interestingly, Type B blood is less common than Type A and O, making it a valuable asset in the world of blood donation and transfusion.
In terms of prevalence, Type B blood varies significantly across different populations. For instance, it is more frequently found in certain ethnic groups, such as those from Asia, compared to others like those from Europe. This geographic variation can influence blood donation strategies and the availability of compatible blood for transfusions. In fact, understanding the distribution of Type B blood can help hospitals and blood banks manage their supplies more effectively.
When it comes to compatibility, individuals with Type B blood can receive blood from Type B and Type O donors. However, it is crucial to avoid transfusions from Type A or AB blood, as the anti-A antibodies present in Type B plasma will react negatively to A antigens, leading to potentially severe immune reactions. Below is a table summarizing the compatibility of Type B blood with other blood types:
| Recipient Type | Compatible Donor Types |
|---|---|
| Type B | Type B, Type O |
| Type B Rh+ | Type B Rh+, Type B Rh-, Type O Rh+, Type O Rh- |
| Type B Rh- | Type B Rh-, Type O Rh- |
Moreover, the implications of having Type B blood extend beyond transfusions. Recent studies have suggested potential links between blood type and certain health conditions, although the evidence is still developing. For instance, some research indicates that individuals with Type B blood may have a different susceptibility to infections or diseases compared to those with other blood types. This area of study is particularly fascinating and underscores the importance of blood type in understanding individual health risks.
In conclusion, Type B blood is not just a label; it represents a complex interplay of genetics, health, and compatibility that is crucial in medical settings. As we continue to explore the mysteries of blood types, it becomes increasingly clear that understanding these differences is essential for providing safe and effective medical care.
- What is the significance of blood type in transfusions? Blood type determines compatibility between donors and recipients, which is critical to prevent adverse reactions during transfusions.
- Can Type B blood donate to other blood types? Type B individuals can donate to other Type B and AB individuals, but not to Type A or O recipients.
- Are there health risks associated with Type B blood? Some studies suggest that individuals with Type B blood may have varying susceptibilities to certain diseases, but more research is needed.

The Rh Factor
The Rh factor is a crucial component in the classification of blood types, determining whether an individual's blood is classified as Rh positive or Rh negative. This classification is primarily based on the presence or absence of the RhD antigen on the surface of red blood cells. If you have the RhD antigen, you are considered Rh positive; if you lack it, you are Rh negative. This distinction is not just a trivial detail; it plays a significant role in various medical scenarios, particularly in blood transfusions and pregnancy.
Understanding the Rh factor is essential for healthcare providers. For instance, during a blood transfusion, receiving Rh-positive blood when you are Rh negative can trigger a severe immune response, leading to complications that can be life-threatening. Thus, the compatibility of Rh factors is as crucial as that of the ABO blood group system. Imagine trying to fit a square peg into a round hole; it just doesn't work, and the consequences can be dire.
In pregnancy, the Rh factor becomes even more critical. An Rh-negative mother carrying an Rh-positive baby can face serious health risks if the baby's Rh-positive blood enters her bloodstream. This situation can lead to a condition known as Rh incompatibility, which can cause hemolytic disease of the newborn (HDN). In this condition, the mother's immune system may produce antibodies that attack the baby's red blood cells, leading to anemia and other complications. Hence, monitoring the Rh status of expectant mothers is vital for ensuring both maternal and fetal health.
To summarize, the Rh factor is not just a label; it has profound implications for health and medical practices. Understanding its significance can lead to better patient outcomes and safer medical procedures. As we delve deeper into the world of blood types, the Rh factor stands out as a pivotal player in the intricate dance of human biology.
- What is the Rh factor? The Rh factor is a protein that can be present on the surface of red blood cells, determining if blood is Rh positive or negative.
- Why is the Rh factor important in pregnancy? An Rh-negative mother carrying an Rh-positive baby can develop antibodies against the baby's blood, leading to serious health issues.
- How can Rh incompatibility be prevented? The administration of Rh immunoglobulin (RhIg) during and after pregnancy can prevent the development of antibodies in Rh-negative mothers.

Rh Positive vs. Rh Negative
The distinction between Rh positive and Rh negative blood types is not just a matter of classification; it plays a pivotal role in various medical scenarios. To put it simply, the Rh factor refers to the presence or absence of the RhD antigen on the surface of red blood cells. If you have this antigen, you are considered Rh positive; if you lack it, you are Rh negative. This seemingly small detail can have significant implications, especially in contexts like blood transfusions and pregnancy.
For instance, if an Rh negative individual receives Rh positive blood, their immune system may recognize the RhD antigen as a foreign invader. This can trigger an immune response, leading to serious complications. This situation is particularly critical during blood transfusions, where compatibility is essential to avoid adverse reactions. The table below summarizes the compatibility of Rh positive and Rh negative blood types:
| Recipient Blood Type | Donor Blood Type | Compatibility |
|---|---|---|
| Rh Positive | Rh Positive | Compatible |
| Rh Positive | Rh Negative | Compatible |
| Rh Negative | Rh Negative | Compatible |
| Rh Negative | Rh Positive | Incompatible |
In the context of pregnancy, the Rh factor takes on even greater significance. If an Rh negative mother is carrying an Rh positive baby, there is a risk of Rh incompatibility. This condition can lead to hemolytic disease of the newborn (HDN), where the mother's immune system attacks the baby's red blood cells. Thankfully, modern medicine has solutions to manage this risk, such as administering Rh immunoglobulin (RhIg) to the mother during pregnancy and after delivery.
Understanding whether you are Rh positive or Rh negative is crucial not only for your health but also for the health of future generations. It’s always a good idea to get tested and keep your healthcare provider informed about your blood type, especially if you’re planning to start a family. The implications of Rh factor compatibility extend beyond just transfusions and pregnancies; they can also influence organ transplant compatibility, making knowledge of your Rh status essential.
- What is the Rh factor? The Rh factor is a protein that can be present on the surface of red blood cells. If you have it, you're Rh positive; if not, you're Rh negative.
- Why is Rh compatibility important during pregnancy? If an Rh negative mother carries an Rh positive baby, it can lead to Rh incompatibility, which may cause serious health issues for the newborn.
- Can Rh negative individuals receive Rh positive blood? No, Rh negative individuals should not receive Rh positive blood due to the risk of an immune response.

Implications for Pregnancy
The Rh factor is a crucial aspect of blood typing that can have significant implications during pregnancy. When a pregnant woman has Rh-negative blood and her baby has Rh-positive blood inherited from the father, it can lead to a condition known as Rh incompatibility. This situation arises because the mother's immune system may recognize the Rh-positive cells as foreign and produce antibodies against them. This immune response can potentially affect the fetus, leading to serious health issues.
One of the most concerning outcomes of Rh incompatibility is a condition called hemolytic disease of the newborn (HDN). In this condition, the antibodies produced by the mother can cross the placenta and attack the baby's red blood cells, leading to anemia, jaundice, and in severe cases, heart failure. It’s essential for expectant mothers to undergo routine blood tests to determine their Rh status early in pregnancy. If an Rh-negative mother is carrying an Rh-positive baby, healthcare providers typically administer a medication called Rho(D) immune globulin to prevent the formation of antibodies against Rh-positive blood cells.
Monitoring and management are crucial in these cases. Regular check-ups can help detect any complications early on. If Rh incompatibility is identified, the healthcare provider may recommend additional treatments or monitoring techniques to ensure the health of both the mother and the baby. In some instances, intrauterine blood transfusions may be necessary to treat the baby before birth.
It's also important to educate expectant parents about the significance of Rh typing. Understanding the implications of Rh factor can empower them to make informed decisions regarding prenatal care. Here are some key points to consider:
- Early testing for Rh factor can prevent complications.
- Rho(D) immune globulin is a preventative measure for Rh-negative mothers.
- Regular monitoring can help manage potential health risks.
In conclusion, the implications of the Rh factor during pregnancy are profound and require careful attention. By being aware of Rh incompatibility and its potential effects, parents can take proactive steps to ensure a healthy pregnancy and delivery.
1. What is Rh incompatibility?
Rh incompatibility occurs when an Rh-negative mother carries an Rh-positive baby, potentially leading to the mother’s immune system attacking the baby's red blood cells.
2. How can Rh incompatibility affect the baby?
It can lead to hemolytic disease of the newborn (HDN), causing anemia and jaundice in the baby, and in severe cases, can be life-threatening.
3. What is Rho(D) immune globulin?
Rho(D) immune globulin is a medication given to Rh-negative mothers to prevent the formation of antibodies against Rh-positive blood cells.
4. When should Rh testing be done during pregnancy?
Rh testing is typically performed during the first prenatal visit, and additional testing may be done later in the pregnancy if needed.
5. Can Rh incompatibility be treated?
Yes, it can be managed with monitoring and treatments such as Rho(D) immune globulin and, in severe cases, intrauterine blood transfusions.

Blood Type Inheritance
Understanding is like piecing together a fascinating puzzle of genetics that reveals how traits are passed from parents to children. Blood types are determined by specific genes inherited from our parents, and this genetic combination ultimately dictates whether we belong to type A, B, AB, or O. Each blood type is associated with different alleles, which are variations of a gene. The ABO blood group system, for example, is controlled by a single gene with three different alleles: A, B, and O. The presence of these alleles in different combinations leads to the various blood types we observe.
When we talk about inheritance, it's essential to consider how these alleles interact. Each person inherits one allele from their mother and one from their father. This means that the possible combinations of alleles can be represented in a simple way:
| Parent 1 Blood Type | Parent 2 Blood Type | Possible Child Blood Types |
|---|---|---|
| A (IAIA or IAi) | A (IAIA or IAi) | A (IAIA, IAi) |
| A (IAIA or IAi) | B (IBIB or IBi) | AB (IAIB), A (IAi), B (IBi) |
| B (IBIB or IBi) | B (IBIB or IBi) | B (IBIB, IBi) |
| O (ii) | A (IAIA or IAi) | A (IAi) |
| O (ii) | B (IBIB or IBi) | B (IBi) |
| O (ii) | O (ii) | O (ii) |
This table illustrates how the blood types of parents can lead to various possible blood types in their children. For instance, if one parent has type A blood and the other has type B, their child could potentially inherit type AB, A, or B blood. However, it’s important to note that the O blood type can only be inherited if at least one parent carries the O allele.
Moreover, the inheritance of the Rh factor, which determines whether blood is positive or negative, follows a similar pattern. Rh positive (Rh+) is dominant over Rh negative (Rh-), meaning that a child will be Rh+ if at least one parent contributes the Rh+ allele. This genetic interplay can result in various combinations, leading to a unique blood type for each individual.
By understanding these genetic principles, parents can make educated guesses about their children's potential blood types, which can be particularly useful in medical situations. Knowledge of blood type inheritance not only helps in anticipating transfusion needs but also plays a role in family planning and understanding potential health issues that may arise due to blood type compatibility.
- Can two O blood type parents have a child with a different blood type? No, two O blood type parents can only have children with O blood type.
- Is it possible for a child to have a different blood type than both parents? Yes, this can occur due to rare genetic mutations or if one parent carries a recessive allele that the other parent does not express.
- How does blood type affect health? Some studies suggest that certain blood types may be linked to varying risks for diseases, but more research is needed in this area.

Understanding Genotypes
Genotypes are the genetic makeup of an individual, determining various traits, including blood type. Each person inherits two alleles for blood type, one from each parent. These alleles can be A, B, or O, and their combination leads to the four primary blood types: A, B, AB, and O. For example, if one parent contributes an A allele and the other a B allele, the resulting genotype would be AB, leading to the AB blood type. This fascinating interplay of genetics is what makes blood types so intriguing.
To put it simply, think of alleles as the letters in a recipe. Just as different combinations of ingredients create unique dishes, different combinations of alleles result in various blood types. Here’s a quick breakdown of how these combinations work:
| Parental Genotypes | Possible Offspring Blood Types |
|---|---|
| AA x AO | A |
| BB x BO | B |
| AB x AO | A, B, AB |
| OO x AO | A, O |
| AB x BO | A, B, AB, O |
These combinations highlight how the inheritance of blood types is not random but rather a predictable outcome based on the genetic contributions from both parents. It's important to note that the O allele is considered recessive, meaning that it will only manifest in the offspring if both parents contribute an O allele. This genetic principle is crucial for understanding why certain blood types may appear more frequently in specific populations.
Moreover, genotypes can also influence other health aspects, such as disease susceptibility. Research has shown that some blood types may be more prone to certain conditions, making understanding genotypes not just a matter of curiosity but a significant aspect of health and medicine.
In summary, understanding genotypes is fundamental to grasping how blood types are inherited. The intricate dance of alleles passed down from parents shapes not only our blood type but also plays a role in our overall health. So next time you think about blood types, remember that there's a rich genetic story behind each one.
- What is the difference between genotype and phenotype?
Genotype refers to the genetic constitution of an individual, while phenotype is the observable physical or biochemical characteristics resulting from the genotype. - Can blood type change over time?
No, blood type is determined by genetics and remains constant throughout a person's life. - How can knowing my blood type help me?
Knowing your blood type is crucial for safe blood transfusions, organ donations, and understanding potential health risks.

Predicting Blood Types in Offspring
When it comes to predicting the blood types of offspring, genetics plays a pivotal role. Understanding how blood types are inherited can be likened to piecing together a puzzle, where each piece represents the genetic contributions from both parents. Blood type inheritance follows specific patterns based on the ABO and Rh systems, which can help parents anticipate their child's blood type with surprising accuracy.
To break it down, each parent contributes one allele from their own blood type. For instance, if one parent has type A blood (genotype AA or AO) and the other has type B blood (genotype BB or BO), the potential blood types of their child could be A, B, AB, or O, depending on the combination of alleles. Here’s a simple representation:
| Parent 1 Blood Type | Parent 2 Blood Type | Possible Offspring Blood Types |
|---|---|---|
| A (AA or AO) | B (BB or BO) | A, B, AB, O |
| A (AA or AO) | O (OO) | A, O |
| B (BB or BO) | O (OO) | B, O |
| AB (AB) | O (OO) | A, B |
Additionally, when considering the Rh factor, if one parent is Rh positive (which can be either Rh+Rh+ or Rh+Rh-) and the other is Rh negative (Rh-Rh-), the child may inherit either Rh positive or Rh negative blood. This is crucial because the Rh status can have significant implications during pregnancy. For example, if an Rh negative mother is carrying an Rh positive baby, it could lead to Rh incompatibility, which is a serious condition that requires medical attention.
Ultimately, predicting blood types in offspring is not just a matter of chance; it’s about understanding the genetic rules at play. By knowing the blood types of both parents, one can calculate the possible blood types of their children, much like forecasting the weather based on atmospheric conditions. This knowledge is not only fascinating but can also be vital for medical reasons, such as planning for blood transfusions or understanding potential health risks associated with certain blood types.
- Can two parents with type O blood have a child with type A or B blood?
No, two type O parents can only have children with type O blood. - What happens if there is an Rh incompatibility during pregnancy?
This can lead to serious health issues for the baby, including hemolytic disease of the newborn, which requires careful monitoring and management. - Are there any blood type combinations that guarantee a specific blood type for the child?
Yes, certain combinations can predict blood types, but there are always exceptions due to the complex nature of genetics.

The Importance of Blood Typing in Medicine
Understanding blood typing is not just a trivial piece of information; it is a critical component of modern medicine. Blood typing is essential in various medical settings, including surgeries, transfusions, and organ transplants. Imagine needing a blood transfusion but receiving the wrong type—this could lead to severe complications, even death. That’s why knowing your blood type can be a lifesaver. It’s like having a secret code that ensures you get the right help when you need it most!
In the realm of transfusions, accurate blood typing can mean the difference between life and death. Before any blood is transfused, healthcare professionals conduct rigorous testing to confirm compatibility. This process involves determining not only the ABO blood group but also the Rh factor. For instance, if a person with Type A blood receives Type B blood, their immune system may react violently, attacking the foreign cells. This reaction can lead to a range of complications, including fever, chills, and even acute kidney failure.
Moreover, blood typing is also crucial in organ transplantation. Just as with transfusions, the compatibility of blood types between donor and recipient plays a significant role in the success of a transplant. If the blood types do not match, the body may reject the organ, leading to serious health issues. To illustrate, here’s a simple table that shows the compatibility of blood types for organ transplants:
| Donor Blood Type | Compatible Recipient Blood Types |
|---|---|
| A | A, AB |
| B | B, AB |
| AB | AB |
| O | A, B, AB, O |
In addition to transfusions and transplants, blood typing also plays a role in diagnostic medicine. For example, certain blood types can influence how patients respond to medications or their susceptibility to certain diseases. By understanding these correlations, doctors can tailor treatments more effectively. It’s like having a personalized medicine plan that’s uniquely suited to your genetic makeup!
Furthermore, blood typing is integral in managing pregnancy. An Rh incompatibility between a mother and her baby can lead to serious complications if not monitored. For example, if an Rh-negative mother is carrying an Rh-positive child, her body might produce antibodies against the baby’s blood. This can lead to conditions such as hemolytic disease of the newborn. Therefore, knowing blood types is essential for expectant mothers to ensure their health and that of their child.
In summary, the importance of blood typing in medicine cannot be overstated. From ensuring safe blood transfusions to successful organ transplants and personalized medical treatments, blood typing is a cornerstone of effective healthcare. It’s a little piece of information that carries a big weight in the world of medicine!
- What is blood typing?
Blood typing is the process of determining an individual's blood group based on the presence of specific antigens on the surface of red blood cells. - Why is blood typing important?
It is crucial for safe blood transfusions, organ transplants, and understanding potential health risks associated with different blood types. - Can blood type affect health?
Yes, certain blood types may be linked to varying susceptibility to diseases and can influence how patients respond to medications. - How is blood type determined?
Blood type is determined through laboratory tests that identify the presence of specific antigens and antibodies in the blood.

Safe Blood Transfusions
When it comes to , the stakes are incredibly high. Each year, millions of people around the world require transfusions due to various medical conditions, surgeries, or traumatic injuries. It’s essential that the blood being transfused is not only of the correct type but also safe for the recipient. The process of ensuring compatibility involves a series of meticulous testing protocols that medical professionals follow rigorously.
Before a transfusion can take place, healthcare providers conduct several tests to determine the recipient's blood type and screen for any potential antibodies that might react negatively with the donor blood. This is critical because receiving incompatible blood can lead to serious, even life-threatening complications. In fact, the immune system may react aggressively against the foreign blood cells, causing a transfusion reaction that can manifest in symptoms ranging from fever and chills to more severe outcomes like kidney failure or shock.
To facilitate safe transfusions, hospitals and blood banks utilize a systematic approach, which includes:
- ABO and Rh Typing: The first step is identifying the ABO blood group and the Rh factor of both the donor and recipient. This ensures that the blood types are compatible.
- Antibody Screening: A sample of the recipient's blood is tested for any unexpected antibodies that could react with the donor blood. This helps to prevent transfusion reactions.
- Crossmatching: This is a crucial test where a small sample of the donor blood is mixed with the recipient's serum to observe any reactions. If no reaction occurs, the blood is considered safe for transfusion.
Furthermore, blood products undergo rigorous screening for infectious diseases, ensuring that any potential pathogens are eliminated before they reach the patient. This is particularly important as blood transfusions can transmit viruses such as HIV, Hepatitis B, and Hepatitis C, among others. Blood banks adhere to strict regulations and guidelines set by health authorities to maintain the highest safety standards.
In addition to these protocols, it’s also vital for patients to communicate openly with their healthcare providers about any previous transfusion reactions or allergies. Such information can significantly influence the choices made regarding blood products and transfusion strategies.
In summary, the journey of a blood transfusion from donor to recipient is a carefully orchestrated process designed to maximize safety and minimize risk. As technology and medical practices continue to evolve, the hope is that these methods will become even more refined, leading to safer and more effective transfusion practices for all patients in need.
- What happens if I receive the wrong blood type? Receiving the wrong blood type can lead to serious complications, including hemolytic reactions, which can be life-threatening.
- How long does a blood transfusion take? A typical blood transfusion can take anywhere from 1 to 4 hours, depending on the type of blood product and the patient's condition.
- Are there risks associated with blood transfusions? Yes, while blood transfusions are generally safe, there are risks involved, including allergic reactions, fever, and, in rare cases, serious complications.
- Can I choose my blood donor? In most cases, you cannot choose your blood donor, as blood is typically collected from volunteer donors and screened for safety.

Organ Transplant Compatibility
When it comes to organ transplants, compatibility is a matter of life and death. The success of a transplant largely depends on the compatibility between the donor and recipient's blood types. This is because the immune system is designed to recognize foreign substances, and if the blood types don’t match, the body may reject the new organ. Understanding the nuances of organ transplant compatibility can save lives and improve outcomes.
In organ transplantation, the ABO blood group system plays a pivotal role. Each blood type has specific antigens, and if the recipient's immune system detects these antigens as foreign, it may trigger an immune response. For example, a person with Type A blood has A antigens and would likely reject an organ from a Type B donor, which has B antigens. This can lead to serious complications, including organ failure. Therefore, blood type compatibility is not just a formality; it is a critical factor in ensuring the transplant's success.
Moreover, the Rh factor adds another layer of complexity. For instance, an Rh-positive recipient can accept organs from both Rh-positive and Rh-negative donors, but the reverse is not true. An Rh-negative recipient should ideally receive an organ from an Rh-negative donor to avoid potential complications. This highlights the importance of thorough testing and matching before any transplant procedure.
| Blood Type | Compatible Donor Blood Types |
|---|---|
| A | A, O |
| B | B, O |
| AB | A, B, AB, O |
| O | O |
In addition to blood type compatibility, other factors such as tissue typing and cross-matching are also essential in the transplant process. Tissue typing assesses the compatibility of human leukocyte antigens (HLAs) between donor and recipient. A closer match can significantly reduce the risk of rejection. Cross-matching is a laboratory test that checks if the recipient's immune system will react against the donor's cells. These tests further refine the compatibility assessment, ensuring that the selected donor organ is the best possible match for the recipient.
The implications of organ transplant compatibility extend beyond the immediate surgical procedure. Successful transplants can lead to improved quality of life and increased life expectancy for recipients. However, mismatched transplants can result in complications that not only affect the organ's function but can also lead to severe health issues, including the need for additional medical interventions or even a second transplant.
As medical science continues to advance, researchers are exploring innovative ways to enhance organ transplant compatibility. Techniques such as gene editing and the use of artificial organs are on the horizon, potentially revolutionizing the field and making it easier to find compatible matches.
In summary, organ transplant compatibility is a multifaceted issue that encompasses blood type matching, tissue typing, and careful cross-matching. Understanding these factors is crucial for both medical professionals and patients alike, as they navigate the complex landscape of organ transplantation.

Future Research on Blood Types
The exploration of blood types is far from over. As science advances, researchers are uncovering new dimensions of how blood types influence not just transfusions and organ transplants, but also our overall health. One of the most exciting areas of future research involves understanding the relationship between blood types and disease susceptibility. For instance, studies have indicated that individuals with certain blood types may have a higher risk of developing particular conditions, such as cardiovascular diseases or infections. This could lead to tailored prevention strategies based on a person's blood type, revolutionizing how we approach health care.
Moreover, advancements in genetic research are opening doors to a more profound understanding of blood types at the molecular level. By examining the genetic markers associated with different blood types, researchers aim to uncover how these markers might affect not only blood compatibility but also how individuals respond to medications. This research could lead to personalized medicine approaches, where treatments are tailored according to a patient's blood type and genetic makeup.
Additionally, the technological advancements in blood typing methods are making it easier and faster to determine blood types with high accuracy. For example, new blood typing technologies utilizing artificial intelligence and machine learning algorithms are being developed. These technologies can analyze blood samples more efficiently, reducing the time required for testing and increasing the reliability of results. This is particularly crucial in emergency situations where every second counts.
Another intriguing avenue of research is the impact of blood types on immune responses. Scientists are investigating how different blood types interact with pathogens and how this interaction can influence the severity of diseases. Understanding these mechanisms could lead to novel therapeutic strategies, enhancing our ability to combat infectious diseases.
As we look towards the future, it is clear that the study of blood types holds immense potential. The implications of this research extend beyond the laboratory; they touch on public health strategies, personalized medicine, and even our understanding of human evolution. The more we learn about blood types, the more we can harness this knowledge to improve health outcomes and tailor medical treatments to individual needs.
- What are the main blood types? The main blood types are A, B, AB, and O, classified based on the presence of specific antigens on red blood cells.
- How can blood type affect health? Research suggests that certain blood types may be linked to varying susceptibility to diseases, influencing health outcomes.
- Why is blood typing important in medicine? Blood typing is crucial for safe transfusions, organ transplants, and ensuring patient compatibility in medical procedures.
- What is the Rh factor? The Rh factor determines whether blood is positive or negative and is significant in pregnancy and transfusions.

Blood Types and Disease Susceptibility
Have you ever wondered why some people seem to catch colds more easily than others? Or why certain diseases appear to affect specific blood types more than others? The intriguing connection between blood types and disease susceptibility has been a topic of research for many years, and recent studies have shed light on this fascinating relationship.
Research suggests that your blood type can influence your body's immune response, potentially affecting how susceptible you are to certain diseases. For example, individuals with Type O blood may have a lower risk of developing certain conditions like cardiovascular diseases, while those with Type A blood might be at a higher risk for infections like H. pylori, which can lead to stomach ulcers. Isn't it astonishing how something as simple as a blood type can play such a significant role in our health?
Here’s a brief overview of how different blood types may correlate with various diseases:
| Blood Type | Associated Diseases |
|---|---|
| Type A | Higher risk of stomach cancer, H. pylori infections |
| Type B | Potentially higher risk of pancreatic cancer |
| Type AB | Increased risk of cognitive decline, heart disease |
| Type O | Lower risk of heart disease, but higher susceptibility to certain infections |
While these associations are compelling, it’s essential to remember that blood type is just one factor among many that contribute to overall health. Genetics, lifestyle choices, and environmental factors also play crucial roles in disease susceptibility. Therefore, if you have a specific blood type, it doesn’t mean you’re destined to develop particular health issues; it merely suggests a potential increased risk.
Moreover, the ongoing research in this area is uncovering more about how blood types interact with various pathogens. For instance, some studies have indicated that blood type may affect how viruses attach to and invade cells. This discovery could have significant implications for developing vaccines and treatments tailored to different blood types, making personalized medicine a reality.
In conclusion, while the link between blood types and disease susceptibility is still being explored, it’s clear that understanding this relationship can enhance our knowledge of health risks and pave the way for more effective medical interventions. So, the next time you think about blood types, remember that they hold secrets about not just who can donate to whom, but also who might be more prone to certain health challenges.
- Can my blood type change over time? No, your blood type remains the same throughout your life, although certain medical conditions can affect blood characteristics.
- Is it possible to determine my blood type at home? Yes, there are blood typing kits available for home use, but for the most accurate results, it's best to consult a medical professional.
- Do blood types affect my diet? Some diet plans suggest that blood type can influence dietary needs, but scientific evidence supporting this claim is limited.
- How can I find out my blood type? You can find out your blood type through a simple blood test at a doctor's office or by using a home testing kit.

Advancements in Blood Typing Technology
In the ever-evolving field of medicine, blood typing technology has made remarkable strides that enhance patient safety and treatment efficacy. Traditional methods of blood typing, which often relied on manual techniques and visual inspections, have now been supplemented or replaced by advanced technologies that offer greater accuracy and speed. One of the most significant advancements is the introduction of automated blood typing systems. These systems utilize sophisticated algorithms and machine learning to analyze blood samples, reducing human error and providing results in a fraction of the time compared to previous methods.
Additionally, the development of microarray technology has revolutionized the way we identify blood group antigens. This method allows for the simultaneous detection of multiple antigens, making it easier to determine a patient's blood type with high precision. Furthermore, the use of DNA-based typing methods has emerged as a powerful tool in blood typing, particularly in complex cases where traditional serological methods may fall short. By analyzing specific genetic markers, these methods can provide definitive results, ensuring that patients receive the correct blood type during transfusions.
Another exciting advancement is the application of point-of-care testing. This technology enables blood typing to be performed at the bedside, allowing for immediate decision-making in critical situations. Imagine a scenario in an emergency room where every second counts; having the ability to quickly and accurately determine a patient's blood type can be lifesaving. This rapid testing capability is bolstered by portable devices that are user-friendly and require minimal training to operate.
Moreover, the integration of cloud-based systems for blood type data management is changing the landscape of transfusion medicine. These systems allow for real-time sharing of blood type information among healthcare providers, ensuring that all parties involved in a patient's care have access to the most current data. This connectivity not only enhances patient safety but also streamlines the transfusion process, reducing waiting times and improving overall efficiency.
As we look to the future, the field of blood typing technology holds even more promise. Ongoing research aims to explore the potential of nanotechnology in blood typing, which could lead to even more sensitive and specific testing methods. The fusion of artificial intelligence with blood typing processes is another frontier that researchers are excited about, as it could lead to predictive analytics that foresee compatibility issues before they arise.
In summary, the advancements in blood typing technology are not just incremental improvements; they represent a paradigm shift in how we approach blood transfusions and patient care. With these innovations, the medical community is better equipped than ever to ensure safe and effective treatments for patients in need.
Frequently Asked Questions
- What are the main blood types?
The main blood types are A, B, AB, and O, classified under the ABO blood group system. Each type is defined by the presence or absence of specific antigens on the surface of red blood cells. For example, Type A has A antigens, Type B has B antigens, Type AB has both, and Type O has neither.
- What is the Rh factor?
The Rh factor is a protein that can be present on the surface of red blood cells. If you have this protein, you're considered Rh positive; if not, you're Rh negative. This distinction is crucial for blood transfusions and during pregnancy, as Rh incompatibility can lead to serious health issues.
- How are blood types inherited?
Blood types are inherited from your parents based on genetic combinations. Each parent contributes one allele, and the combination determines your blood type. For instance, if one parent has Type A and the other has Type B, their child could potentially have Type A, B, AB, or O, depending on the specific alleles inherited.
- Why is blood typing important in medicine?
Blood typing is vital in medicine for ensuring safe blood transfusions, organ transplants, and various surgical procedures. Knowing a patient's blood type helps prevent adverse reactions during transfusions and is also essential for matching organ donors with recipients.
- Can blood types affect disease susceptibility?
Yes, some studies suggest that certain blood types may be linked to varying susceptibility to specific diseases. For example, research has indicated that individuals with Type O blood might have a lower risk of certain infections, while other blood types could be more prone to different health conditions.
- What are the compatibility rules for blood transfusions?
For safe blood transfusions, compatibility is key. Generally, Type A can receive A or O, Type B can receive B or O, Type AB can receive all types (A, B, AB, O), and Type O can only receive O. Additionally, Rh positive individuals can receive Rh positive or negative blood, while Rh negative individuals should only receive Rh negative blood.
- How does blood typing technology work?
Modern blood typing technology involves various methods, including serological tests that identify blood group antigens and antibodies. These tests are crucial for ensuring accuracy and safety in blood transfusions and organ transplants, helping to prevent potentially life-threatening reactions.