The Biology of Allergies - How They Develop and Can Be Managed
Allergies, though often dismissed as mere inconveniences, can significantly impact the quality of life for millions of people around the world. Understanding the biology behind these reactions is essential not only for those affected but also for families and communities seeking to support their loved ones. This article dives into the intricate mechanisms of allergies, exploring how they develop, the role of the immune system, and effective management strategies. By the end of this read, you’ll have a clearer picture of allergies and how to tackle them head-on.
At the core of every allergic reaction is a group of substances known as allergens. These are typically harmless to most people, but for those with allergies, they can trigger a cascade of immune responses. Common allergens include pollen, dust mites, mold spores, pet dander, and certain foods. Imagine walking through a beautiful park in spring, only to be met with a sneeze-inducing cloud of pollen. For allergy sufferers, this isn’t just a minor annoyance; it can lead to serious discomfort and health issues.
Allergens can be found in various places, from the air we breathe to the food we consume. When a susceptible individual encounters an allergen, their immune system mistakenly identifies it as a threat, leading to an exaggerated response. This section will explore the sources of common allergens and how they provoke immune responses, setting the stage for understanding the biological underpinnings of allergies.
The immune system is our body’s defense mechanism, designed to protect us from harmful invaders like bacteria and viruses. However, in the case of allergies, this system can go awry. When an allergen enters the body, the immune system identifies it and mounts a response that can sometimes be disproportionate. This is where the role of Immunoglobulin E (IgE) antibodies comes into play.
IgE antibodies are a specific type of antibody that play a central role in allergic reactions. When a person with allergies is exposed to an allergen, their immune system produces IgE antibodies that latch onto the allergen. This process not only signals the immune system to react but also prepares the body for future encounters with the same allergen. Think of it as the immune system creating a 'wanted poster' for the allergen, ensuring that it’s recognized in the future.
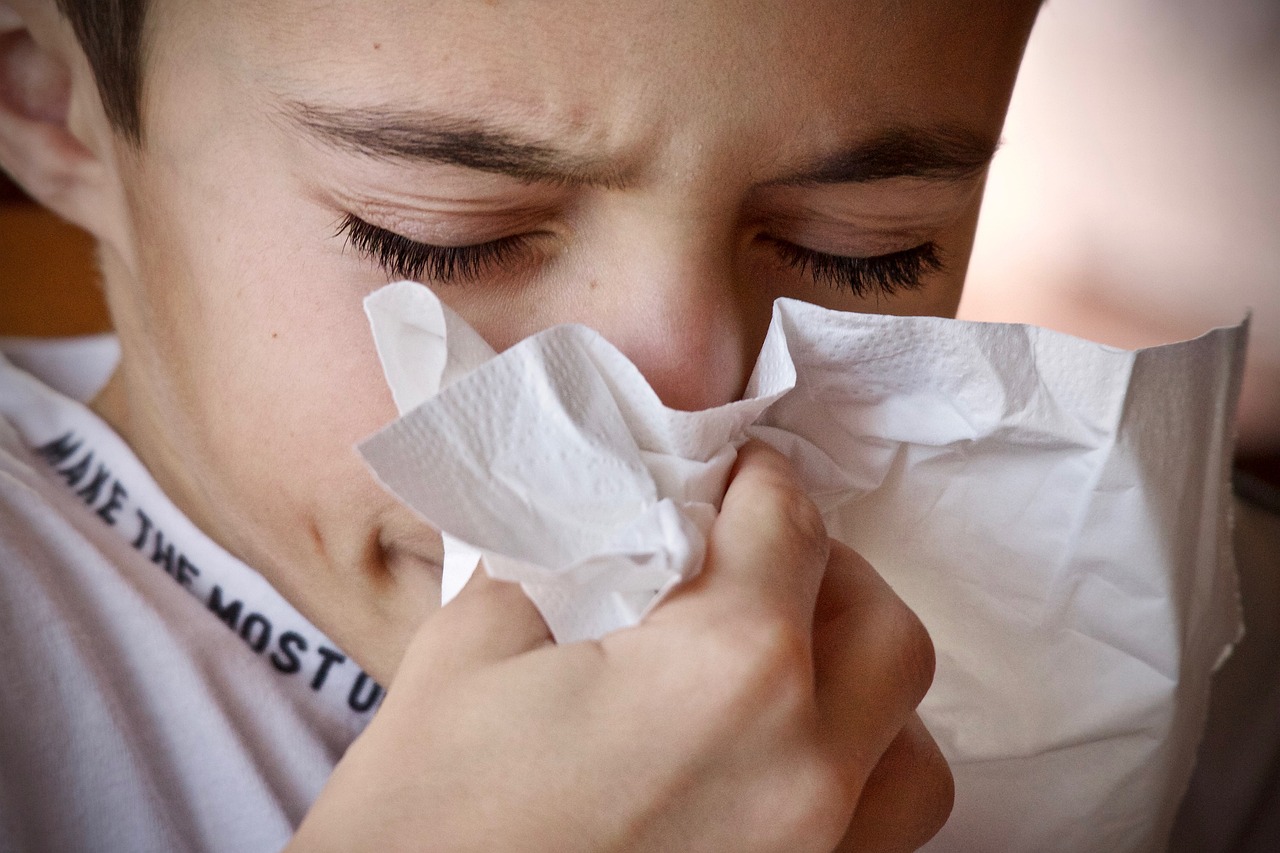
Once IgE antibodies are produced, they attach themselves to specialized immune cells known as mast cells. Upon subsequent exposure to the same allergen, these mast cells release histamines and other chemicals, leading to the classic symptoms of allergies—sneezing, itching, and swelling. This activation process is akin to setting off a fire alarm; once triggered, it alerts the entire neighborhood, causing a rush of activity and sometimes chaos.
The inflammatory response is another crucial aspect of allergies. When mast cells release histamines, it initiates a cascade of events involving various immune mediators, including cytokines. These substances amplify the immune response, leading to increased blood flow and swelling in the affected areas. This is why allergy symptoms can feel so overwhelming—your body is essentially in a state of alarm, responding vigorously to what it perceives as a threat.
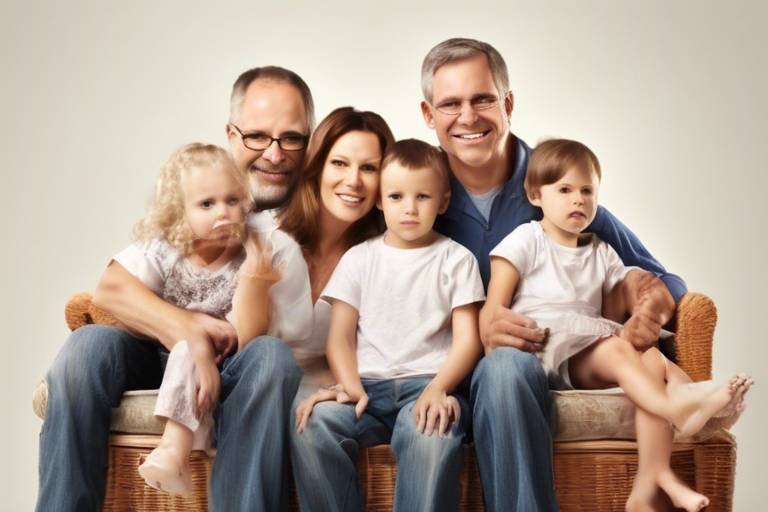
It’s fascinating to note that genetics can significantly influence who develops allergies. If you have a family history of allergies, your chances of experiencing them increase. This hereditary component means that allergies can run in families, making it essential for parents to be aware of their children’s potential risk. Understanding these genetic factors can help families navigate allergy management more effectively.
While genetics plays a role, environmental factors are often the catalysts for allergic reactions. Common triggers include pollen, dust mites, mold, and pet dander. These allergens are prevalent in our surroundings, making it crucial to identify and manage them. For instance, pollen counts can soar during certain seasons, leading to an uptick in allergic reactions among sensitive individuals.
Seasonal allergies, often referred to as hay fever, are a prime example of how environmental factors trigger allergic responses. During spring and fall, pollen from trees, grasses, and weeds can wreak havoc on allergy sufferers. Symptoms may include sneezing, nasal congestion, and itchy eyes, making it challenging to enjoy the outdoors. Managing these allergies often involves staying indoors during peak pollen times and using air purifiers to reduce exposure.
Indoor allergens, such as dust mites and pet dander, can be just as troublesome. These allergens thrive in our homes, making it essential to implement strategies to minimize exposure. Regular cleaning, using hypoallergenic bedding, and maintaining low humidity levels can significantly reduce the presence of these triggers. Remember, a clean home is often a happy home for allergy sufferers!
Effectively managing allergies is crucial for improving one’s quality of life. Various strategies can help alleviate symptoms, including avoidance techniques, medications, and lifestyle changes. Understanding these options empowers individuals to take control of their health and well-being.
Several medications are available to treat allergies, each with its benefits and potential side effects. Antihistamines can provide quick relief from symptoms, while corticosteroids can help reduce inflammation. It’s essential to consult with a healthcare provider to find the best treatment plan tailored to individual needs.
For those seeking long-term relief, allergy immunotherapy may be an option. This treatment involves gradually exposing the individual to increasing amounts of the allergen, helping the body build a tolerance over time. While it requires commitment and patience, many find it to be an effective solution for managing allergies.
- What are the most common allergens? Common allergens include pollen, dust mites, mold, pet dander, and certain foods.
- How can I tell if I have allergies? Symptoms often include sneezing, itching, nasal congestion, and skin rashes. Consulting a healthcare provider can provide a definitive diagnosis.
- Are allergies hereditary? Yes, allergies can run in families, and having a family history increases the likelihood of developing them.
- What is the best way to manage allergies? Effective management may involve avoiding allergens, using medications, and considering treatments like allergy immunotherapy.

Understanding Allergens
Allergens are those pesky substances that can turn a perfectly good day into a sneeze-fest. But what exactly are they? Simply put, allergens are typically harmless substances that trigger an exaggerated immune response in certain individuals. This response can lead to a variety of uncomfortable symptoms, ranging from mild irritations to severe reactions. Common allergens can be found all around us, and understanding them is the first step towards managing allergies effectively.
Some of the most common allergens include:
- Pollen: This is a major trigger for seasonal allergies, especially during spring when plants release their reproductive particles into the air.
- Dust mites: These microscopic creatures thrive in our homes, particularly in bedding, carpets, and upholstered furniture, making them a common indoor allergen.
- Pet dander: Proteins found in the skin flakes, saliva, and urine of furry friends can cause allergic reactions in sensitive individuals.
- Mold spores: Mold can grow in damp areas of the home and release spores that can be inhaled, leading to allergic reactions.
- Food allergens: Certain foods, such as peanuts, tree nuts, milk, eggs, and shellfish, can provoke severe allergic reactions in some people.
When an allergen enters the body of a susceptible person, it can trigger the immune system to react as if it were a harmful invader. This is where the magic—and often chaos—begins. The immune system mistakenly identifies the allergen as a threat and starts producing specific antibodies known as Immunoglobulin E (IgE). This process is akin to a fire alarm going off in a building; once triggered, everyone reacts, often in a panic.
Once IgE antibodies are produced, they attach themselves to certain cells in the body, particularly mast cells. These mast cells are like little sentinels, always on the lookout for invaders. When they encounter their specific allergen, they release a cocktail of chemicals, including histamines, which are responsible for the symptoms we associate with allergies, such as sneezing, itching, and swelling. It’s like a chain reaction that spirals out of control, leading to the various symptoms that can disrupt daily life.
Understanding the sources of allergens and how they affect individuals is crucial for anyone dealing with allergies. It's not just about knowing what to avoid; it’s also about recognizing the signs of an allergic reaction and knowing how to respond. For instance, if you’re aware that pollen is high during certain times of the year, you can take proactive measures like staying indoors or using air purifiers to reduce exposure.
In summary, allergens are everywhere, and they come in many forms. By understanding what they are and how they work, individuals can better prepare themselves to manage their allergies effectively. This knowledge empowers people to take control of their environments and improve their quality of life, turning the tide against those pesky allergens.
The Immune System's Role
When we think about allergies, the immune system often takes center stage. It’s like a vigilant security guard, constantly on the lookout for potential threats. But what happens when this guard mistakenly identifies harmless substances, like pollen or pet dander, as dangerous intruders? This misidentification is the crux of allergic reactions. The immune system's primary role is to protect the body from harmful pathogens, but in individuals with allergies, it can go into overdrive, leading to a cascade of symptoms that can be quite uncomfortable.
At the heart of this process are specialized cells and proteins that work together to mount an immune response. When an allergen is encountered, the immune system responds by producing specific antibodies known as Immunoglobulin E (IgE). These antibodies are like the alarm bells, signaling the body that there’s an intruder. The production of IgE is a significant step in the allergy development process and plays a pivotal role in how the body reacts to allergens.
Once IgE antibodies are produced, they attach themselves to mast cells and basophils, which are types of white blood cells. Imagine these cells as highly trained soldiers, ready to spring into action at a moment's notice. Upon subsequent exposure to the same allergen, these cells release a variety of chemicals, including histamines, which are responsible for many of the symptoms associated with allergic reactions. This can lead to a range of symptoms from sneezing and itching to more severe reactions like anaphylaxis.
The activation of mast cells is a critical part of the allergic response. When an allergen binds to the IgE on the surface of these cells, it triggers them to release histamines and other inflammatory mediators. This process can be likened to setting off a firework; the initial spark leads to a rapid and widespread explosion of symptoms throughout the body. These symptoms can include:
- Itching
- Swelling
- Redness
- Difficulty breathing
As histamines flood the bloodstream, they cause blood vessels to dilate and become more permeable, leading to the classic signs of inflammation. This is why you might experience a runny nose or watery eyes during allergy season; your body is responding as if it's under attack.
The inflammatory response is a complex series of events that occurs when the immune system detects an allergen. It involves various immune mediators, including cytokines, which are signaling proteins that help regulate immunity and inflammation. These cytokines can amplify the immune response, leading to even more severe symptoms. Think of cytokines as the loudspeakers at a concert, amplifying every sound to ensure everyone hears the message loud and clear. This amplification can sometimes lead to chronic inflammation, which is a persistent state of heightened immune response, causing long-term issues for individuals with allergies.
Understanding the immune system's role in allergies is crucial for developing effective management strategies. By recognizing how the body reacts to allergens, individuals can take proactive steps to minimize their exposure and manage their symptoms more effectively. Whether it’s through medication, lifestyle changes, or avoidance strategies, being informed is the first step towards better managing allergies.
Q: What are common symptoms of allergies?
A: Common symptoms include sneezing, itching, nasal congestion, skin rashes, and in severe cases, difficulty breathing.
Q: Can allergies be cured?
A: While there is no cure for allergies, they can often be managed effectively with medication and lifestyle adjustments.
Q: How can I identify my specific allergens?
A: Allergy testing, such as skin prick tests or blood tests, can help identify specific allergens that trigger your symptoms.

IgE Antibodies
Immunoglobulin E (IgE) antibodies are like the alarm system of our immune system when it comes to allergies. Imagine your body as a fortress, and IgE antibodies are the guards on the lookout for intruders—those pesky allergens that can cause chaos. When a person with allergies encounters an allergen, their immune system mistakenly identifies it as a threat, triggering the production of IgE antibodies. This response is fascinating yet perplexing, as it reveals how our bodies can sometimes overreact to harmless substances.
These antibodies are primarily produced by a type of immune cell known as B cells. Once produced, IgE antibodies bind to allergens and attach themselves to mast cells and basophils, which are another type of immune cell. This attachment is crucial because it sets the stage for the fireworks that follow when the allergen reappears. When the body encounters the same allergen again, the IgE antibodies signal mast cells to release chemicals like histamine, which lead to the symptoms commonly associated with allergic reactions, such as sneezing, itching, and swelling.
To give you a clearer picture, here's a simple overview of how IgE antibodies function:
| Step | Description |
|---|---|
| 1 | Allergen Exposure: The body comes into contact with an allergen. |
| 2 | IgE Production: The immune system produces IgE antibodies in response. |
| 3 | Binding: IgE antibodies bind to mast cells and basophils. |
| 4 | Subsequent Exposure: When re-exposed to the allergen, IgE triggers mast cells to release histamine. |
| 5 | Allergic Reaction: Histamine release leads to allergy symptoms. |
This process can be likened to a fire alarm system in a building. Initially, the alarm might not go off when smoke is detected (the first exposure to an allergen), but once the alarm is set (IgE antibodies are produced), any subsequent smoke (allergen exposure) will trigger a loud alarm (allergic reaction). This often results in a range of symptoms that can vary from mild to severe, depending on the individual and the allergen involved.
Interestingly, not everyone produces IgE antibodies in response to allergens. Some people may have a different immune response, which can lead to varying degrees of allergic reactions. This variability is why allergies can be so unpredictable and why some individuals may have severe reactions while others may only experience mild discomfort.
Understanding the role of IgE antibodies is crucial for developing effective allergy management strategies. By targeting this immune response, healthcare providers can help patients find relief and improve their quality of life. Whether through medications that block histamine or immunotherapy that gradually desensitizes the immune system to allergens, there are ways to manage the effects of these overzealous antibodies.
- What are IgE antibodies? IgE antibodies are a type of antibody produced by the immune system in response to allergens, playing a key role in allergic reactions.
- How do IgE antibodies cause allergic reactions? When allergens are encountered, IgE antibodies trigger mast cells to release histamine, leading to allergy symptoms.
- Can everyone have IgE antibodies? No, not everyone produces IgE antibodies in response to allergens, which is why allergic reactions can vary widely among individuals.
- How can allergies be managed? Allergies can be managed through avoidance of allergens, medications, and immunotherapy.

Activation of Mast Cells
Mast cells are like the body’s alarm system, lying in wait throughout the tissues, ready to spring into action when they encounter an allergen. When you come into contact with something you’re allergic to—be it pollen, pet dander, or certain foods—these cells become activated. But how does this process work? It all begins when an allergen binds to the specific IgE antibodies that are attached to the surface of mast cells. This binding is akin to a key fitting into a lock, triggering a cascade of events that lead to the release of various chemicals.
Once activated, mast cells release a variety of mediators, the most notable of which is histamine. Histamine is responsible for many of the classic symptoms associated with allergic reactions, such as itching, swelling, and redness. Imagine histamine as a firework going off in your body, causing a spectacular but unwelcome display of symptoms. The release of histamine leads to increased blood flow and permeability of blood vessels, which can cause swelling and inflammation in the affected areas.
In addition to histamine, mast cells release other mediators such as cytokines and leukotrienes, which further amplify the inflammatory response. Cytokines act as signaling molecules that recruit additional immune cells to the site of the allergen exposure, perpetuating the allergic reaction. This is where the situation can escalate, as more immune cells flood the area, leading to heightened symptoms. You might think of this as a snowball effect—once it starts rolling, it just keeps getting bigger and bigger!
Understanding the activation of mast cells is crucial for developing effective treatments for allergies. By targeting the processes involved in mast cell activation and mediator release, researchers and healthcare professionals can create therapies that help mitigate allergic reactions. For instance, medications such as antihistamines work by blocking the action of histamine, effectively putting a damper on the fireworks and helping to alleviate symptoms.
In summary, the activation of mast cells is a pivotal moment in the allergy response. It’s a complex interplay of biological mechanisms that can lead to a range of symptoms, from mild discomfort to severe reactions. Recognizing how these cells function not only helps us understand allergies better but also lays the groundwork for effective management strategies.
- What are mast cells? Mast cells are immune cells that play a crucial role in allergic reactions by releasing histamine and other mediators upon activation.
- How do mast cells get activated? Mast cells are activated when allergens bind to IgE antibodies on their surface, triggering the release of chemicals that cause allergy symptoms.
- What symptoms are caused by mast cell activation? Symptoms can include itching, swelling, redness, and other allergic reactions, depending on the site of activation.
- Can mast cell activation be prevented? While it may not be possible to prevent activation entirely, understanding triggers and using medications can help manage symptoms effectively.
Inflammatory Response
The is a vital and complex biological process that occurs when the body encounters an allergen. When an allergen invades the body, the immune system reacts by triggering a series of events designed to eliminate the perceived threat. This response is not just a simple reaction; it is a well-orchestrated dance involving various cells and signaling molecules that work together to protect the body. Think of it as a fire alarm system: when the alarm goes off, the firefighters (immune cells) rush to the scene to contain the fire (the allergen).
During an allergic reaction, the body releases a variety of cytokines and other immune mediators that play crucial roles in inflammation. These substances signal other immune cells to come to the site of the allergen exposure, leading to swelling, redness, and discomfort. The inflammatory response can be likened to a double-edged sword; while it is essential for fighting off allergens and pathogens, it can also cause significant distress and symptoms in individuals who are sensitive to these triggers.
Here’s a brief overview of the key components involved in the inflammatory response:
- Cytokines: These are signaling proteins that mediate and regulate immunity, inflammation, and hematopoiesis. They are crucial in orchestrating the inflammatory response.
- Mast Cells: These cells are found in connective tissues and release histamines during an allergic reaction, which contributes to inflammation and typical allergy symptoms.
- Histamines: These compounds increase blood vessel permeability and promote the movement of immune cells to the site of inflammation, leading to swelling and redness.
- Other Immune Mediators: Various other cells and proteins, including eosinophils and leukotrienes, participate in the inflammatory response, amplifying the reaction and prolonging symptoms.
The inflammatory response can manifest in various ways, depending on the individual and the allergen involved. Common symptoms include itching, swelling, redness, and sometimes even severe reactions like anaphylaxis. Understanding this response is not only crucial for those suffering from allergies but also for healthcare providers aiming to offer effective treatment options. By managing inflammation, patients can significantly improve their quality of life and reduce the frequency of allergic reactions.
- What causes the inflammatory response in allergies? The inflammatory response is triggered when the immune system mistakenly identifies harmless substances (allergens) as threats, leading to the release of various immune mediators.
- How can I manage my inflammatory response to allergens? Management strategies include avoiding known allergens, using antihistamines to reduce symptoms, and consulting with healthcare professionals for tailored treatment plans.
- Can the inflammatory response lead to chronic issues? Yes, repeated inflammatory responses can lead to chronic conditions such as asthma or allergic rhinitis, making it crucial to manage allergies effectively.

Genetic Factors in Allergies
When it comes to allergies, the old saying "it's in your genes" rings remarkably true. Genetic factors play a pivotal role in determining who develops allergies and who remains blissfully unaffected. Research indicates that if one or both parents have allergies, their children are significantly more likely to inherit this predisposition. But how does this genetic influence work?
At the heart of this genetic connection is the complex interplay between multiple genes and environmental factors. Scientists have identified various genes associated with the immune response, particularly those involved in the production of Immunoglobulin E (IgE) antibodies. These antibodies are crucial in mediating allergic reactions, and their overproduction is often linked to genetic susceptibility. For instance, variations in the IL-4 gene can lead to increased IgE production, heightening the risk of developing allergies.
Moreover, it's not just about the presence of certain genes; it's also about how they interact with the environment. This is where the concept of the “hygiene hypothesis” comes into play. This theory suggests that a lack of early childhood exposure to infectious agents, microorganisms, and parasites can lead to an increased risk of allergies. Essentially, our immune systems need challenges to develop properly, and a sterile environment may hinder this process.
To better understand the genetic factors contributing to allergies, researchers often look at family histories and conduct studies involving twins. These studies reveal that identical twins, who share nearly 100% of their genetic makeup, are more likely to both develop allergies compared to fraternal twins, who share only about 50% of their genes. This strong correlation underscores the significant role genetics play in allergic conditions.
Here’s a quick overview of some key genetic factors associated with allergies:
- Family History: A strong predictor of allergy development.
- Gene Variants: Certain gene variations can increase the likelihood of allergies.
- Immune System Regulation: Genes that affect immune responses can heighten allergy susceptibility.
Understanding these genetic factors is crucial not only for individuals but also for healthcare professionals. By recognizing the hereditary nature of allergies, doctors can better assess risk factors and provide tailored advice for families. This knowledge can empower families to take preventive measures, such as reducing exposure to known allergens or considering genetic counseling.
As we delve deeper into the science of allergies, it becomes increasingly clear that genetics is just one piece of a larger puzzle. While we can’t change our genetic makeup, awareness of these factors can help us navigate the world of allergies more effectively. So, whether you're battling seasonal sniffles or indoor irritants, understanding your genetic predisposition can be a game-changer in managing your symptoms.
Q: Can allergies be inherited?
A: Yes, allergies can run in families. If one or both parents have allergies, their children are at a higher risk of developing them.
Q: What role do environmental factors play?
A: Environmental factors, such as exposure to allergens and infections, interact with genetic predispositions to influence allergy development.
Q: Is it possible to prevent allergies if they run in the family?
A: While you can't change your genetics, you can take preventive steps, such as minimizing exposure to known allergens during childhood.

Environmental Triggers
When we think about allergies, we often picture sneezing, itchy eyes, or even skin rashes. But what really causes these reactions? The answer lies in our environment. are substances in our surroundings that can provoke allergic reactions in susceptible individuals. These triggers can be as common as the air we breathe or as hidden as the dust lurking in our homes. Understanding these triggers is essential for managing allergies effectively.
One of the most notorious culprits is pollen. During certain seasons, trees, grasses, and weeds release tiny grains into the air to fertilize other plants. For many, this natural process becomes a nightmare. The pollen count can soar, leading to a surge in allergy symptoms. Did you know that different plants release pollen at different times of the year? This seasonal variation means that some individuals may only suffer during specific months, while others might be affected year-round.
Another common environmental trigger is dust mites. These microscopic creatures thrive in warm, humid conditions and are often found in bedding, carpets, and upholstered furniture. They feed on dead skin cells, which we shed daily. For those allergic to dust mites, exposure can lead to persistent symptoms such as sneezing, runny nose, and even asthma attacks. Keeping your home clean and dry can significantly reduce dust mite populations, but it’s not always easy. Regular vacuuming and washing bedding in hot water can help, but it requires consistent effort.
Pet dander is another significant trigger. While our furry friends bring joy and companionship, they also shed tiny flakes of skin, saliva, and urine that can provoke allergic reactions. Even if you don't have pets, visiting a friend or family member with animals can trigger symptoms. It's important to note that some breeds are marketed as hypoallergenic, but no breed is entirely free of allergens. If you’re considering bringing a pet into your home, think about your allergy history and potential reactions.
Moreover, mold spores can also contribute to allergic reactions. Mold thrives in damp areas, such as bathrooms, basements, and around leaky pipes. When mold spores become airborne, they can be inhaled, triggering symptoms in sensitive individuals. Keeping humidity levels low and ensuring proper ventilation can help prevent mold growth. If you notice a musty smell or visible mold, it’s crucial to address it promptly to avoid exacerbating allergy symptoms.
To sum it up, environmental triggers play a pivotal role in allergy development. By recognizing these triggers, you can take proactive steps to minimize exposure and manage symptoms effectively. Remember, it’s not just about avoiding allergens; it’s also about understanding how they interact with your body. Knowledge is power, and in the battle against allergies, it can make all the difference.
- What are the most common environmental allergens?
The most common environmental allergens include pollen, dust mites, pet dander, and mold spores.
- How can I reduce exposure to allergens in my home?
Regular cleaning, using air purifiers, and maintaining low humidity levels can help reduce allergen exposure.
- Are there any treatments for environmental allergies?
Yes, treatments include antihistamines, corticosteroids, and allergy immunotherapy, which can help manage symptoms.
- Can environmental allergies be prevented?
While you can't always prevent allergies, you can manage exposure to known triggers and maintain a clean living environment.

Seasonal Allergies
Ah, the beauty of spring! Flowers bloom, trees regain their lush green, and the world seems to come alive. But for many, this vibrant season is accompanied by a less-than-welcome guest: . Also known as hay fever, these allergies can turn the joys of warmer weather into a sneezy, itchy nightmare. So, what exactly causes these pesky reactions, and how can we manage them?
Seasonal allergies are primarily triggered by pollen, which is released by trees, grasses, and weeds during specific times of the year. Each type of pollen has its own season. For instance, tree pollen typically peaks in early spring, while grass pollen is more prevalent in late spring to early summer. Weeds, on the other hand, often contribute to allergies in late summer and fall. This cyclical pattern means that individuals with seasonal allergies often find themselves battling symptoms at different times throughout the year.
When pollen enters the body, it can provoke an immune response in sensitive individuals. The immune system mistakenly identifies pollen as a harmful substance, leading to the production of IgE antibodies. These antibodies then trigger the release of histamines and other chemicals, resulting in the familiar symptoms of seasonal allergies:
- Runny or stuffy nose
- Itchy or watery eyes
- Sneezing
- Coughing
- Fatigue
For those who suffer from seasonal allergies, the symptoms can feel overwhelming, almost like having a constant cold. It’s crucial to recognize when allergy season is approaching. Keeping track of local pollen counts can help you prepare. Many weather apps and websites provide daily pollen forecasts, allowing you to plan outdoor activities accordingly.
But fear not! There are several effective management strategies to help alleviate the symptoms of seasonal allergies. First and foremost, avoidance is key. Here are some tips to reduce your exposure to pollen:
- Stay indoors during peak pollen times, usually in the early morning.
- Keep windows closed to prevent pollen from entering your home.
- Use air purifiers with HEPA filters to trap allergens.
- Shower and change clothes after spending time outdoors to wash away pollen.
Additionally, medications can provide relief. Over-the-counter antihistamines, nasal corticosteroids, and decongestants are commonly used to combat allergy symptoms. However, it’s always best to consult with a healthcare professional to determine the most suitable treatment for your specific needs.
In some cases, individuals may benefit from allergy immunotherapy. This long-term treatment option gradually desensitizes the immune system to specific allergens, potentially reducing the severity of allergic reactions over time. While it requires commitment and patience, many find it to be a game-changer in managing their seasonal allergies.
In summary, while seasonal allergies can be a nuisance, understanding their triggers and implementing effective management strategies can significantly improve your quality of life. So, as you step outside to enjoy the beauty of nature, arm yourself with knowledge and tools to combat those pesky allergens!
Here are some common questions regarding seasonal allergies:
- What are the most common allergens during spring? Tree pollen is the primary culprit in spring, followed by grass pollen as the season progresses.
- Can seasonal allergies cause fatigue? Yes, the body's immune response to allergens can lead to fatigue, especially if symptoms disrupt sleep.
- Are there any natural remedies for seasonal allergies? Some people find relief with natural remedies such as saline nasal rinses, local honey, or certain herbal supplements, but it's important to consult a healthcare provider before trying new treatments.

Indoor Allergens
Indoor allergens are a significant concern for many individuals, especially those who suffer from allergies. These allergens can be found in various places within our homes and workplaces, often lurking in the most unexpected corners. Common culprits include dust mites, pet dander, mold spores, and even pollen that sneaks in through open windows. Understanding these allergens is crucial for managing symptoms and creating a more comfortable living environment.
Dust mites, microscopic creatures that thrive in warm, humid environments, are among the most prevalent indoor allergens. They feed on dead skin cells, which we shed daily, and are commonly found in bedding, upholstered furniture, and carpets. In fact, a typical bed can harbor thousands of these tiny pests! Their waste products are what trigger allergic reactions, leading to symptoms such as sneezing, itchy eyes, and nasal congestion.
Another common indoor allergen is pet dander, which consists of tiny flakes of skin shed by cats, dogs, and other furry animals. Even if you're not a pet owner, dander can still find its way into your home through clothing or by visiting friends or family with pets. The proteins in pet dander can cause severe reactions in sensitive individuals, making it essential to consider pet ownership carefully.
Mold is another significant indoor allergen that thrives in damp, poorly ventilated areas. It can grow on walls, ceilings, and even in your bathroom. The spores released by mold can become airborne, making them easy to inhale and potentially leading to respiratory issues. Regular cleaning and maintaining low humidity levels in your home can help keep mold at bay.
To combat these indoor allergens effectively, here are some practical tips:
- Regular Cleaning: Frequent vacuuming and dusting can significantly reduce dust mites and dander. Using a vacuum with a HEPA filter is highly recommended.
- Wash Bedding Weekly: Wash sheets, pillowcases, and blankets in hot water (at least 130°F) to kill dust mites.
- Control Humidity: Keep humidity levels below 50% using dehumidifiers or air conditioners, as this can help prevent mold growth.
- Air Purifiers: Consider using HEPA air purifiers to capture airborne allergens, particularly in bedrooms and living areas.
By being proactive and implementing these strategies, you can significantly reduce your exposure to indoor allergens and improve your overall quality of life. Remember, a little effort can go a long way in creating a healthier, allergy-free environment.
1. What are the most common indoor allergens?
The most common indoor allergens include dust mites, pet dander, mold spores, and pollen. These allergens can trigger allergic reactions in sensitive individuals.
2. How can I reduce dust mites in my home?
To reduce dust mites, regularly clean your home, wash bedding in hot water weekly, and use allergen-proof covers on pillows and mattresses.
3. Is it possible to be allergic to mold?
Yes, many people are allergic to mold. Mold spores can trigger respiratory issues and other allergic reactions, especially in damp environments.
4. Can air purifiers help with indoor allergens?
Yes, HEPA air purifiers can effectively capture airborne allergens, reducing their concentration in your home and helping alleviate allergy symptoms.

Management Strategies
Managing allergies effectively is crucial for enhancing the quality of life for those affected. With the right strategies, individuals can minimize their exposure to allergens and alleviate their symptoms. One of the primary approaches to managing allergies is through avoidance techniques. This means identifying the specific allergens that trigger reactions and taking steps to limit contact with them. For example, if pollen is a known trigger, staying indoors during high pollen counts can be beneficial. Similarly, for those allergic to dust mites, regularly washing bedding in hot water and using dust-proof covers on pillows and mattresses can significantly reduce exposure.
In addition to avoidance, many people turn to medications to help manage their symptoms. There is a range of options available that can provide relief. Antihistamines are commonly used to counteract the effects of histamines released during an allergic reaction. These medications come in various forms, including pills, liquids, and nasal sprays. Corticosteroids are another option, often prescribed to reduce inflammation associated with allergies. While these medications can be effective, it's important to consult with a healthcare professional to understand their benefits and potential side effects.
Another promising approach to allergy management is allergy immunotherapy. This long-term treatment involves gradually exposing the patient to increasing amounts of the allergen, aiming to desensitize the immune system over time. Patients who undergo immunotherapy often report a significant reduction in their allergy symptoms after completing the treatment course. It’s essential to discuss this option with an allergist, as they can provide tailored advice based on individual health profiles and allergy severity.
Moreover, lifestyle changes can play a pivotal role in managing allergies. Simple modifications such as maintaining a clean living environment, using air purifiers, and avoiding smoking can contribute to a significant decrease in allergic reactions. It's also beneficial to keep track of local pollen forecasts and mold counts, especially for those with seasonal allergies. By being proactive and informed, individuals can better navigate their allergy challenges.
To summarize, effective management of allergies involves a combination of avoidance strategies, medication, immunotherapy, and lifestyle adjustments. Each person’s experience with allergies is unique, and what works for one individual may not work for another. Therefore, it’s crucial to work closely with healthcare providers to develop a personalized management plan that addresses specific needs and circumstances.
- What are the most common types of allergies? Allergies can be triggered by a variety of substances, including pollen, dust mites, pet dander, mold, and certain foods.
- How do I know if I have an allergy? Symptoms like sneezing, itching, rashes, and difficulty breathing may indicate an allergy. Consulting an allergist for testing is the best way to confirm.
- Can allergies go away on their own? Some allergies can diminish over time, especially in children, but many individuals may continue to experience symptoms throughout their lives.
- Is there a cure for allergies? While there is no definitive cure, effective management strategies can help control symptoms and improve quality of life.

Medications for Allergies
When it comes to managing allergies, the right medications can make a world of difference. Whether you're dealing with sneezing, itching, or other uncomfortable symptoms, understanding your options is key to finding relief. So, what are the most common types of medications available for allergies, and how do they work?
First off, we have antihistamines. These are often the go-to choice for many allergy sufferers. They work by blocking histamine, a chemical that your body releases during an allergic reaction. This means that when you take an antihistamine, it can help reduce symptoms like runny noses, sneezing, and itchy eyes. Some popular over-the-counter options include cetirizine (Zyrtec), loratadine (Claritin), and diphenhydramine (Benadryl). However, be cautious! While antihistamines can be effective, some may cause drowsiness, so it's essential to read labels carefully.
Next in line are corticosteroids. These are usually prescribed for more severe allergy symptoms, especially when it comes to nasal congestion. Corticosteroid nasal sprays, such as fluticasone (Flonase) and mometasone (Nasonex), can significantly reduce inflammation in the nasal passages, leading to easier breathing and less discomfort. They are not immediate relief solutions but can provide long-term control when used consistently.
Another option worth mentioning is leukotriene receptor antagonists, like montelukast (Singulair). These medications work by blocking leukotrienes, which are chemicals in the immune system that contribute to allergic reactions. They can be particularly effective for individuals with asthma and allergies, making them a versatile choice for those who experience both conditions.
For those who prefer a more targeted approach, decongestants can provide quick relief from nasal congestion. Medications such as pseudoephedrine (Sudafed) work by constricting blood vessels in the nasal passages, reducing swelling and congestion. However, they should be used with caution, as they can raise blood pressure and may not be suitable for everyone.
In some cases, individuals may benefit from allergy shots, also known as immunotherapy. This long-term treatment involves gradually exposing the patient to small amounts of allergens, helping the immune system build tolerance over time. While it requires a commitment of time and effort, many find it to be a game changer in managing their allergies.
It's important to remember that while medications can provide relief, they are most effective when combined with lifestyle changes and avoidance strategies. For example, keeping windows closed during high pollen seasons, using air purifiers, and regularly cleaning your living space can help reduce your exposure to allergens.
In summary, understanding the various medications available for allergies can empower you to take control of your symptoms. Whether you opt for antihistamines, corticosteroids, or other treatments, consulting with a healthcare provider is essential to find the best plan tailored to your specific needs.
- What are the side effects of antihistamines? Some common side effects include drowsiness, dry mouth, and dizziness. Always check with your doctor if you experience any severe reactions.
- Can I take multiple allergy medications at once? It's crucial to consult with a healthcare provider before combining medications to avoid potential interactions.
- How long does it take for allergy medications to work? Antihistamines can start working within an hour, while corticosteroids may take several days to show full effects.
- Are there natural remedies for allergies? Some people find relief using natural remedies like nasal saline rinses, local honey, and herbal supplements, but these should be discussed with a healthcare professional.

Allergy Immunotherapy
Allergy immunotherapy, often referred to as allergy shots or sublingual tablets, is a long-term treatment designed to reduce the severity of allergic reactions. Unlike standard medications that merely alleviate symptoms, immunotherapy addresses the underlying cause of allergies by gradually desensitizing the immune system to specific allergens. This process can be likened to training a dog to respond to commands; over time, the immune system learns to tolerate the allergens instead of overreacting to them.
During the treatment, patients receive small doses of the allergen, which are gradually increased over time. This method helps the immune system become accustomed to the allergen, thereby reducing the intensity of the allergic response. The treatment typically involves two phases:
- Build-up Phase: This initial phase lasts for several months and involves frequent injections or doses of the allergen to build up the body’s tolerance.
- Maintenance Phase: Once the desired dose is reached, patients enter the maintenance phase, which lasts for several years and requires less frequent doses.
Immunotherapy is particularly effective for common allergens such as pollen, dust mites, and pet dander. It has been shown to provide long-lasting relief, even after the treatment has concluded. Studies indicate that approximately 80% of patients experience significant improvement in their allergy symptoms, which can lead to a better quality of life. However, it's essential to note that this treatment may not be suitable for everyone. Individuals with certain health conditions or those who are pregnant should consult their healthcare provider before starting immunotherapy.
One of the most significant advantages of allergy immunotherapy is its potential to prevent the development of new allergies and the progression of allergic diseases, such as asthma. By addressing the root cause, immunotherapy not only alleviates symptoms but also helps to promote long-term health benefits.
As with any medical treatment, there are some risks associated with immunotherapy. Patients might experience local reactions at the injection site, such as swelling or redness, and in rare cases, more severe allergic reactions can occur. Therefore, it’s crucial to have these treatments administered by a qualified healthcare professional who can monitor for any adverse reactions.
In conclusion, allergy immunotherapy represents a promising avenue for those struggling with persistent allergies. By committing to this treatment, patients can potentially reclaim their lives from the burden of allergies, enjoying activities and environments that were once off-limits. If you think you might be a candidate for immunotherapy, consult with an allergist to explore your options and develop a personalized treatment plan.
- How long does allergy immunotherapy take to work? It typically takes several months to see significant improvement, with full benefits often realized after 1-2 years of treatment.
- Is allergy immunotherapy safe? Yes, when administered by a trained professional, it is generally safe, although some individuals may experience mild side effects.
- Can immunotherapy cure allergies? While it may not cure allergies entirely, it can significantly reduce symptoms and improve quality of life.
- How often do I need to go for treatment? During the build-up phase, visits may be weekly or biweekly, while maintenance doses are typically given every few weeks to months.
Frequently Asked Questions
- What are common allergens that trigger allergic reactions?
Common allergens include pollen, dust mites, pet dander, mold, and certain foods like nuts, shellfish, and dairy. These substances can provoke strong immune responses in sensitive individuals, leading to various symptoms.
- How does the immune system react to allergens?
When an allergen enters the body, the immune system mistakenly identifies it as a threat. This triggers the production of IgE antibodies, which bind to mast cells. Upon subsequent exposure to the same allergen, these mast cells release histamines and other chemicals, causing allergy symptoms.
- What role do genetic factors play in allergies?
Genetics can significantly influence a person's likelihood of developing allergies. If one or both parents have allergies, their children are more likely to experience similar sensitivities, highlighting the hereditary nature of these conditions.
- What are seasonal allergies, and how can they be managed?
Seasonal allergies, often referred to as hay fever, occur during specific times of the year when pollen counts are high. Management strategies include staying indoors on high pollen days, using air purifiers, and taking antihistamines to alleviate symptoms.
- What are some effective management strategies for allergies?
Effective management strategies include avoiding known allergens, using over-the-counter or prescription medications, and considering allergy immunotherapy. Lifestyle changes, such as keeping living spaces clean and reducing exposure to triggers, can also help.
- What medications are commonly used to treat allergies?
Common medications for allergies include antihistamines, which relieve symptoms like sneezing and itching, and corticosteroids, which reduce inflammation. It's essential to consult a healthcare provider to determine the best treatment option for individual needs.
- What is allergy immunotherapy, and how does it work?
Allergy immunotherapy is a long-term treatment that involves gradually exposing the patient to increasing amounts of the allergen. This process helps the immune system build tolerance, potentially leading to long-lasting relief from allergy symptoms.