The Future of Digital Innovation in Healthcare
The world of healthcare is witnessing a revolution like never before, driven by the relentless march of digital innovation. From telemedicine to artificial intelligence, these advancements are not merely trends; they are transformative forces that are reshaping how patients receive care and how healthcare providers operate. Imagine a world where your doctor is just a click away, where medical diagnoses can be made in seconds, and where wearable devices keep track of your health in real-time. This isn't science fiction—this is the reality we are stepping into.
As we delve deeper into the intricacies of digital innovation, it's essential to understand that these technologies are more than just tools; they are lifelines that enhance patient care and streamline health management. The integration of digital solutions in healthcare is not only improving efficiency but also fostering a more personalized approach to medicine. Patients are becoming more empowered, taking charge of their health through technology that provides them with information and support at their fingertips.
However, with great power comes great responsibility. As we embrace these innovations, we must also grapple with challenges such as data privacy, regulatory hurdles, and the need for equitable access to technology. The future of digital healthcare hinges on our ability to navigate these complexities while maximizing the benefits of these advancements. In this article, we will explore the various facets of digital innovation in healthcare, shedding light on its impact, the challenges it presents, and the exciting future that lies ahead.
Telemedicine has emerged as a vital service in healthcare, offering remote consultations and monitoring that break down geographical barriers. The growth of telemedicine has been nothing short of astounding, particularly in the wake of the COVID-19 pandemic, which accelerated its adoption. Patients can now connect with healthcare providers from the comfort of their homes, making it easier for those in rural areas or with mobility issues to access medical care. This accessibility is crucial as it enhances patient engagement and encourages timely interventions.
One of the most significant benefits of telemedicine is its ability to deliver care efficiently. Patients can schedule virtual appointments, reducing wait times and eliminating the need for travel. Moreover, telemedicine platforms often include features such as secure messaging, video consultations, and remote monitoring, allowing for comprehensive care management. However, despite its advantages, telemedicine also faces challenges, including technological barriers and concerns about the quality of care delivered remotely.
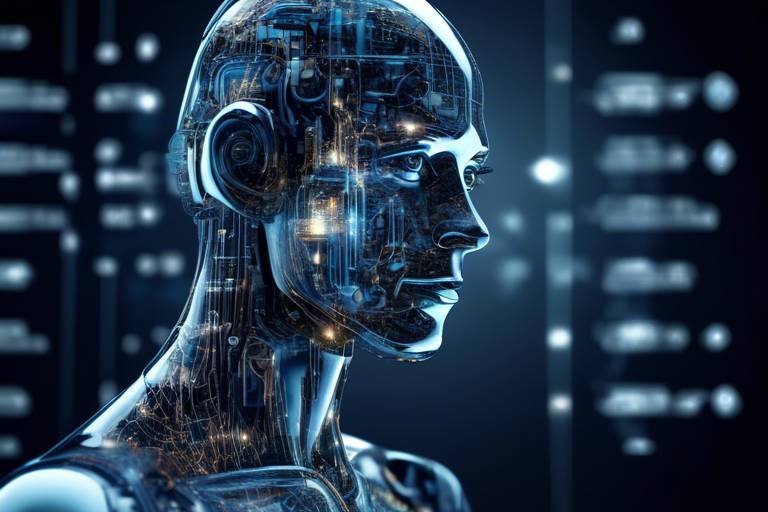
Artificial intelligence (AI) is revolutionizing diagnostics by improving accuracy and speed in disease detection. AI tools are being integrated into healthcare systems to assist in diagnosing conditions that may have previously gone unnoticed. Imagine a world where a machine can analyze thousands of medical images in seconds, identifying anomalies that a human eye might miss. This is the power of AI in diagnostics, and it is changing the way healthcare providers approach patient care.
Machine learning algorithms play a crucial role in analyzing vast amounts of medical data. These algorithms can sift through electronic health records, lab results, and imaging studies to identify patterns that help predict patient outcomes. For example, by analyzing historical data, machine learning can help doctors tailor treatment plans to individual patients, enhancing the effectiveness of interventions. The potential for personalized medicine is immense, and as these technologies evolve, we can expect even more sophisticated applications in the future.
However, the use of AI raises important data privacy issues. The ethical considerations surrounding patient data security are paramount, as healthcare providers must ensure that sensitive information is protected from breaches and misuse. Patients must feel confident that their data is handled with care and that their privacy is respected. As we integrate AI into healthcare, robust measures must be in place to safeguard patient information.
As AI applications expand, regulatory challenges arise. The need for guidelines and standards to ensure safe and effective AI use in healthcare cannot be overstated. Regulatory bodies must work closely with technology developers to create frameworks that promote innovation while protecting patients. This balance is critical to the successful integration of AI into healthcare.
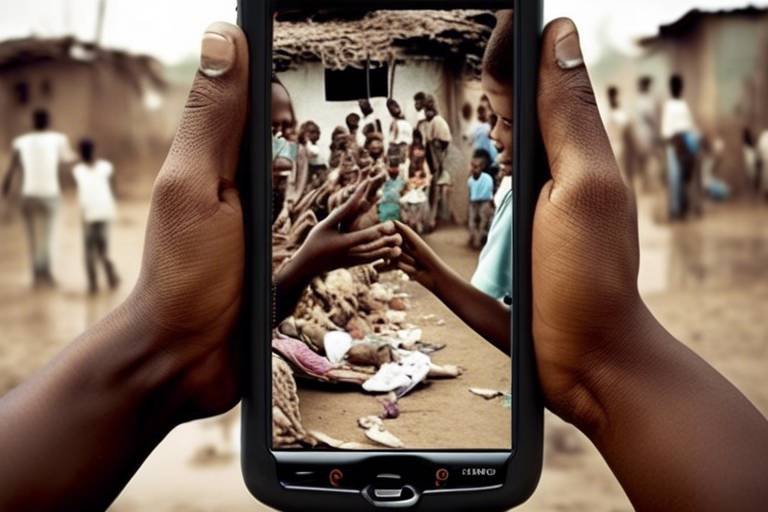
Telehealth is making healthcare more accessible, particularly in rural areas. It is a game changer for healthcare equity, ensuring that individuals who may have previously faced barriers to access can now receive the care they need. However, challenges remain, including the digital divide, which affects those without reliable internet access or technological literacy. Addressing these barriers is essential to ensure that the benefits of telehealth reach all segments of the population.
Wearable devices are changing how patients monitor their health. From smartwatches that track heart rates to fitness bands that monitor activity levels, these technologies empower individuals to take charge of their health in unprecedented ways. Imagine having a personal health assistant on your wrist, providing real-time feedback and alerts that can help you make healthier choices.
Integrating wearable technology with existing health systems enhances data collection and patient management. This integration allows healthcare providers to access real-time data, enabling them to make informed decisions about patient care. However, challenges such as data interoperability and security concerns must be addressed to realize the full potential of this integration.
The future of wearable technology in healthcare promises even more innovations. Emerging trends such as advanced biometric sensors, AI-driven analytics, and seamless integration with telehealth platforms will further empower patients to manage their health. As these technologies evolve, we can expect to see a shift towards preventive care, where individuals can identify health issues before they become serious.
- What is telemedicine?
Telemedicine refers to the remote diagnosis and treatment of patients through telecommunications technology. - How does AI improve diagnostics?
AI enhances diagnostics by analyzing large datasets quickly and accurately, identifying patterns that may be missed by human providers. - What are the benefits of wearable health technology?
Wearable devices enable continuous health monitoring, empower patients to take charge of their health, and facilitate early detection of potential health issues. - What are the challenges of integrating technology in healthcare?
Challenges include data privacy concerns, regulatory hurdles, and ensuring equitable access to technology.

Telemedicine Revolution
In recent years, telemedicine has surged into the spotlight, transforming the way healthcare is delivered. Imagine being able to consult with a doctor from the comfort of your own home, without the hassle of waiting rooms or long commutes. This is no longer a futuristic dream; it's a reality that many patients are now experiencing. The growth of telemedicine has been nothing short of explosive, particularly in light of recent global health challenges that have pushed both patients and providers to embrace remote healthcare solutions.
One of the most significant benefits of telemedicine is its ability to enhance patient access to medical professionals. For individuals living in rural or underserved areas, accessing healthcare can be a daunting task. Long distances to clinics, limited transportation options, and a shortage of healthcare providers often create barriers to receiving timely care. Telemedicine breaks down these barriers by allowing patients to connect with healthcare providers through video calls, phone consultations, or even messaging platforms. This not only saves time but also ensures that patients receive the care they need when they need it.
Moreover, telemedicine has proven invaluable during emergencies, such as the COVID-19 pandemic. With hospitals overwhelmed, patients could still consult healthcare professionals without risking exposure to the virus. This adaptability has highlighted the importance of having robust telemedicine services in place. As we look to the future, it’s clear that telemedicine will play a pivotal role in how healthcare is provided.
However, the rise of telemedicine isn’t without its challenges. While the technology is advancing rapidly, there are still issues that need addressing, such as the digital divide. Not everyone has the necessary technology or internet access to take advantage of telemedicine services. Additionally, some patients may feel uncomfortable using technology for their healthcare needs, preferring face-to-face interactions. Healthcare providers must find ways to bridge these gaps to ensure that telemedicine is accessible to all.
As we move forward, it’s essential to consider the regulatory landscape surrounding telemedicine. Policies and reimbursement structures are evolving, but they must keep pace with the rapid advancements in technology. Ensuring that telemedicine is covered by insurance and that providers are adequately compensated for their services is crucial for its long-term success.
In summary, the telemedicine revolution is transforming healthcare in remarkable ways. By improving accessibility, enhancing patient experience, and adapting to emergencies, telemedicine is reshaping the future of healthcare delivery. As we continue to innovate and address the challenges that come with this transformation, the potential for telemedicine to improve patient outcomes is boundless.

Artificial Intelligence in Diagnostics
Artificial Intelligence (AI) is not just a buzzword; it’s a game-changer in the realm of diagnostics. Imagine walking into a clinic where a machine can analyze your symptoms and medical history within seconds, providing a diagnosis that is both accurate and quick. This is no longer science fiction; it's happening right now! The integration of AI into healthcare systems is revolutionizing how we approach disease detection and treatment planning, making the process more efficient and reliable.
One of the most significant advantages of AI in diagnostics is its ability to process vast amounts of data rapidly. Traditional diagnostic methods can be time-consuming, often requiring multiple tests and consultations. In contrast, AI algorithms can sift through medical records, lab results, and even genetic information to identify patterns that may be missed by human eyes. For instance, AI systems can analyze imaging scans for signs of tumors or fractures with remarkable precision. This capability not only enhances the accuracy of diagnoses but also reduces the time patients spend waiting for results, which can be crucial in time-sensitive situations.
Moreover, AI tools are constantly learning and evolving. With each case they analyze, they become more adept at recognizing symptoms and predicting outcomes. This is where machine learning algorithms come into play. These algorithms are designed to improve over time, making them invaluable in a field where knowledge is continuously expanding. They can help healthcare professionals make informed decisions about treatment plans tailored to individual patients. For example, AI can suggest personalized medication regimens based on a patient’s unique genetic makeup and health history, which can lead to better outcomes and fewer side effects.
Machine learning algorithms are the backbone of AI in diagnostics. They analyze historical data and learn from it, allowing them to make predictions about future outcomes. This capability is particularly useful in predicting patient outcomes, such as the likelihood of recovery from a specific condition or the potential for complications during treatment. The ability to forecast these outcomes can significantly enhance patient care, allowing healthcare providers to intervene early and adjust treatment plans as necessary.
| Machine Learning Algorithm | Application in Diagnostics |
|---|---|
| Support Vector Machines | Classifying medical images and detecting anomalies. |
| Neural Networks | Analyzing complex patterns in data, such as genetic information. |
| Decision Trees | Helping clinicians make decisions based on patient data. |
However, with great power comes great responsibility. The use of AI in diagnostics raises important data privacy concerns. As these systems require access to sensitive patient information, ensuring the security of this data is paramount. Healthcare providers must navigate the ethical considerations of using AI while maintaining patient trust. Additionally, regulatory challenges are emerging as AI applications expand, necessitating guidelines and standards to ensure safe and effective use in healthcare settings.
In conclusion, the integration of AI into diagnostics is paving the way for a more efficient, accurate, and personalized healthcare experience. As technology continues to advance, the potential for AI to transform patient care is limitless. Staying informed about these developments is crucial for both healthcare professionals and patients alike, ensuring that we harness the full potential of AI while addressing the challenges it brings.
- How does AI improve diagnostic accuracy? AI analyzes vast datasets to identify patterns and anomalies that may not be visible to the human eye, leading to more accurate diagnoses.
- What are the ethical concerns surrounding AI in healthcare? Concerns include patient data privacy, consent, and the potential for bias in AI algorithms.
- Can AI replace human doctors? While AI can assist in diagnostics, it is not intended to replace human doctors; rather, it serves as a tool to enhance their capabilities.
- How is AI integrated into current healthcare systems? AI tools are being integrated into electronic health records (EHRs), imaging systems, and decision support systems to streamline processes and improve patient outcomes.

Machine Learning Algorithms
Machine learning algorithms are like the unsung heroes of the healthcare industry, tirelessly sifting through mountains of medical data to uncover insights that can change lives. Imagine having a super-smart assistant who can analyze thousands of patient records in seconds, identifying patterns and predicting outcomes with remarkable accuracy. This is the power of machine learning in action, and it’s revolutionizing the way we approach patient care.
These algorithms utilize vast datasets, often referred to as big data, to learn from past experiences and improve their performance over time. For instance, they can analyze symptoms, lab results, and even genetic information to help healthcare professionals make more informed decisions. The implications are staggering; by harnessing the predictive capabilities of machine learning, doctors can tailor treatments to individual patients, effectively personalizing healthcare like never before.
One of the most exciting aspects of machine learning is its ability to predict patient outcomes. For example, algorithms can assess a patient's risk of developing conditions such as diabetes or heart disease by evaluating lifestyle factors, family history, and other health indicators. This predictive power enables early interventions, potentially saving lives and reducing healthcare costs. Here’s a quick breakdown of how machine learning algorithms are being applied in various healthcare scenarios:
| Application | Description |
|---|---|
| Disease Prediction | Identifying patients at risk for chronic diseases through data analysis. |
| Treatment Personalization | Customizing treatment plans based on individual patient data. |
| Resource Allocation | Optimizing hospital resources by predicting patient admissions. |
| Clinical Decision Support | Assisting healthcare providers in making evidence-based decisions. |
However, while the benefits are clear, the integration of machine learning algorithms into healthcare systems is not without its challenges. Data quality is paramount; if the data fed into these algorithms is flawed or biased, the outcomes can be misleading. Moreover, the need for transparency in how these algorithms make decisions is critical, as healthcare professionals and patients alike must trust the recommendations provided by these systems.
As we look to the future, the potential of machine learning in healthcare is boundless. Continuous advancements in computational power and data collection methods will only enhance the capabilities of these algorithms. Imagine a future where your wearable device not only tracks your health metrics but also communicates with a machine learning model that predicts your health trajectory, prompting you to make lifestyle changes before issues arise. This is not just a dream; it’s a glimpse into the future of personalized medicine.
- What are machine learning algorithms? Machine learning algorithms are computational models that learn from data to make predictions or decisions without being explicitly programmed.
- How do machine learning algorithms improve patient outcomes? By analyzing large datasets, these algorithms can identify patterns and predict health risks, allowing for early interventions and personalized treatment plans.
- What challenges do machine learning algorithms face in healthcare? Key challenges include data quality, algorithm transparency, and the need for regulatory frameworks to ensure safe and effective use.

Data Privacy Concerns
In the rapidly evolving landscape of digital healthcare, data privacy has emerged as a critical concern. As healthcare providers increasingly rely on artificial intelligence (AI) to analyze patient data, the risk of exposing sensitive information grows. Imagine your personal health records—filled with intimate details about your medical history—being accessed by unauthorized individuals. It’s a nightmare scenario that many patients fear, and rightly so. The integration of AI in diagnostics and treatment planning necessitates robust measures to ensure that patient data remains confidential and secure.
The ethical implications of using AI in healthcare are vast. With algorithms processing vast amounts of data, there is a potential for misuse or mishandling of information. For instance, if a healthcare provider uses AI to predict patient outcomes but fails to secure the data, it could lead to breaches that compromise patient privacy. This situation raises the question: how can we trust technology if we cannot trust the systems that protect our most personal information? The answer lies in establishing stringent data protection protocols that prioritize patient confidentiality.
Moreover, healthcare organizations must comply with various regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, which sets national standards for the protection of health information. However, as technology advances, so do the methods of potential breaches. Cybersecurity threats are becoming increasingly sophisticated, and healthcare providers must stay one step ahead. This is where the importance of continuous training and education for staff comes into play. They need to be well-versed in data protection practices to mitigate risks effectively.
To address these concerns, several measures can be implemented:
- Data Encryption: Encrypting sensitive data ensures that even if it is intercepted, it remains unreadable to unauthorized users.
- Access Controls: Limiting access to patient data only to those who need it for legitimate purposes can significantly reduce the risk of breaches.
- Regular Audits: Conducting frequent audits of data access and usage can help identify potential vulnerabilities and rectify them promptly.
In conclusion, while the integration of AI in healthcare brings numerous benefits, the associated data privacy concerns cannot be overlooked. It is imperative for healthcare organizations to adopt a proactive approach in safeguarding patient information, ensuring that trust remains at the forefront of the patient-provider relationship. After all, in a world where technology is intertwined with our health, maintaining privacy is not just a legal obligation—it’s a moral one.
- What are the main data privacy concerns in healthcare?
Data privacy concerns in healthcare primarily revolve around unauthorized access to sensitive patient information, potential data breaches, and the ethical use of AI technologies. - How can healthcare organizations protect patient data?
Organizations can protect patient data through measures such as data encryption, implementing strict access controls, and conducting regular audits to monitor data usage. - What regulations govern data privacy in healthcare?
In the United States, HIPAA sets national standards for the protection of health information, but other regulations may apply depending on the region and specific circumstances.

Regulatory Challenges
The rapid expansion of artificial intelligence (AI) in healthcare brings with it a host of that need to be addressed to ensure safe and effective use. As AI technologies become more integrated into healthcare systems, governing bodies are faced with the complex task of creating regulations that not only protect patients but also foster innovation. The challenge lies in striking a balance between ensuring patient safety and allowing for the flexibility necessary for advancements in technology.
One of the primary concerns is the lack of standardized guidelines for AI applications. Different countries and regions have varying regulations, which can lead to confusion and inconsistency in implementation. For instance, while some countries may allow AI-driven diagnostics to be used without extensive pre-market testing, others may require rigorous validation processes that can delay the deployment of beneficial technologies. This disparity can hinder global collaboration and slow down the pace of innovation.
Furthermore, accountability is a significant issue in the realm of AI. If an AI system fails to provide an accurate diagnosis or treatment recommendation, who is held responsible? Is it the developers of the AI, the healthcare providers who utilize it, or the institutions that implement it? These questions highlight the need for clear regulations that delineate responsibilities and liabilities in the event of an error. Establishing a framework for accountability is crucial to building trust among patients and healthcare professionals alike.
Data privacy is another critical regulatory challenge. With AI systems relying on vast amounts of patient data to function effectively, ensuring the security of this information is paramount. Regulatory bodies must create stringent guidelines to protect sensitive patient information from breaches and misuse. This includes implementing robust data encryption methods, secure storage solutions, and strict access controls. Failure to safeguard patient data not only compromises individual privacy but can also lead to severe legal repercussions for healthcare providers.
In addition, there is a pressing need for ongoing education and training for healthcare professionals regarding AI technologies. As these tools become more prevalent, practitioners must understand how to use them effectively and ethically. Regulatory frameworks should include provisions for training programs that equip healthcare providers with the knowledge needed to navigate the complexities of AI in their practice. This will not only enhance patient care but also ensure that AI is used responsibly and ethically.
In summary, while the potential of AI in healthcare is immense, the regulatory challenges it presents cannot be overlooked. Policymakers must work collaboratively with technology developers, healthcare providers, and other stakeholders to create a comprehensive regulatory framework that addresses these challenges. By doing so, we can unlock the full potential of AI while ensuring the safety and well-being of patients.
- What are the main regulatory challenges facing AI in healthcare? Regulatory challenges include the lack of standardized guidelines, accountability issues, data privacy concerns, and the need for ongoing education for healthcare professionals.
- Why is accountability important in AI healthcare applications? Accountability is crucial to determine who is responsible in case of errors, which helps build trust among patients and healthcare providers.
- How can data privacy be ensured with AI technologies? Regulatory bodies can enforce stringent guidelines for data encryption, secure storage, and strict access controls to protect sensitive patient information.
- What role does education play in the successful implementation of AI in healthcare? Education ensures that healthcare professionals are equipped with the necessary knowledge to use AI technologies effectively and ethically, improving patient care.

Telehealth Accessibility
In recent years, has emerged as a game-changer in the healthcare landscape, particularly for individuals living in rural or underserved areas. Imagine a world where you can consult with your doctor from the comfort of your home, avoiding long travel times and waiting rooms filled with sick patients. That’s the reality that telehealth brings to the table! By leveraging technology, telehealth has made it possible for patients to access medical care without the traditional barriers.
One of the most significant benefits of telehealth is its ability to bridge the gap between patients and healthcare providers. For many, especially those in remote locations, getting to a hospital or clinic can be a daunting task. Telehealth services allow patients to connect with healthcare professionals through video calls, phone consultations, and even messaging platforms. This not only saves time but also reduces the stress associated with in-person visits. The convenience it offers can lead to better patient engagement and adherence to treatment plans.
However, while telehealth is making strides in accessibility, it’s essential to recognize that not everyone has equal access to these services. Factors such as internet connectivity, technological literacy, and availability of devices can create barriers for certain populations. For instance, older adults may struggle with using technology, while low-income families might lack the necessary internet access to take advantage of telehealth services. It’s crucial for healthcare systems to address these disparities to ensure that telehealth can truly benefit everyone.
To illustrate the impact of telehealth accessibility, consider the following table that highlights the challenges faced by various demographics:
| Demographic Group | Challenges |
|---|---|
| Rural Patients | Limited internet connectivity and long travel distances to healthcare facilities. |
| Low-Income Families | Lack of access to devices and high-speed internet. |
| Older Adults | Technological literacy and comfort with digital platforms. |
| Minority Communities | Language barriers and cultural differences in healthcare perceptions. |
Addressing these challenges is crucial for the future of telehealth. Policymakers, healthcare providers, and technology companies must collaborate to develop solutions that enhance accessibility. This could involve initiatives like providing subsidized internet access, offering training programs for older adults, or creating multilingual telehealth platforms to cater to diverse populations.
In conclusion, while telehealth has made remarkable progress in enhancing healthcare accessibility, there is still much work to be done. By acknowledging and addressing the barriers that exist, we can ensure that telehealth is not just a privilege for some, but a right for all. The future of healthcare should be inclusive, and telehealth is a vital step in that direction.
- What is telehealth? Telehealth refers to the use of digital information and communication technologies to access healthcare services remotely.
- How does telehealth improve accessibility? Telehealth allows patients to consult with healthcare providers without needing to travel, making it easier for those in remote areas to receive care.
- What challenges does telehealth face? Challenges include internet connectivity issues, technological literacy, and disparities in access among different demographic groups.
- Are telehealth services covered by insurance? Many insurance plans cover telehealth services, but coverage can vary by provider and location.

Wearable Health Technology
In recent years, has taken the healthcare world by storm. These innovative devices, ranging from fitness trackers to smartwatches, are no longer just trendy gadgets; they are becoming essential tools for monitoring and managing health. Imagine having a personal health assistant right on your wrist, constantly tracking your heart rate, sleep patterns, and even stress levels! This transformation is not just about convenience; it's about empowering individuals to take charge of their health like never before.
One of the most exciting aspects of wearable technology is its ability to provide real-time data. For instance, devices equipped with sensors can monitor vital signs and send alerts if something seems off. This capability can be a game-changer for those with chronic conditions, as it allows for immediate intervention when necessary. Think of it as having a virtual safety net that keeps you informed and connected to your healthcare providers. With the right data at their fingertips, doctors can make more informed decisions about treatment plans, ultimately improving patient outcomes.
Moreover, the integration of wearable devices with existing health systems is paving the way for a more cohesive approach to healthcare. When data collected from wearables is seamlessly shared with healthcare providers, it enhances the overall patient experience. Imagine visiting your doctor and having all your health metrics readily available, allowing for more personalized and effective care. However, this integration is not without its challenges. Issues such as data compatibility and privacy concerns need to be addressed to ensure that the technology is both effective and secure.
As we look to the future, the potential for wearable health technology seems limitless. Emerging trends suggest that we will see even more advanced features in the coming years. For example, some devices are already being developed to monitor blood glucose levels non-invasively. This could revolutionize diabetes management, providing patients with continuous insights without the discomfort of traditional blood tests. Additionally, the incorporation of artificial intelligence in wearables could lead to predictive analytics, where devices not only track health metrics but also anticipate potential health issues before they arise.
In summary, wearable health technology is not just a passing fad; it's a fundamental shift in how we approach health and wellness. By harnessing the power of data and technology, we can create a more proactive and personalized healthcare experience. As these devices continue to evolve, they hold the promise of transforming lives and improving health outcomes for countless individuals.
- What types of wearable health technology are available? Wearable health technology includes fitness trackers, smartwatches, heart rate monitors, and sleep trackers, among others.
- How can wearable devices improve my health? They provide real-time data on your health metrics, allowing for better monitoring and management of chronic conditions.
- Are there privacy concerns with wearable health technology? Yes, data privacy is a significant concern, and it's essential to choose devices that prioritize user data security.
- Can wearable technology replace regular doctor visits? While wearables can enhance health monitoring, they are not a substitute for professional medical advice and regular check-ups.

Integration with Health Systems
As we dive deeper into the realm of wearable health technology, one of the most exciting developments is the integration of these devices with existing health systems. Imagine a world where your smartwatch not only tracks your steps but also communicates directly with your doctor’s office, sharing vital health data in real-time. This seamless connection can lead to better patient management and more personalized care, transforming how we approach health and wellness.
However, integrating wearable technology into health systems is not without its challenges. There are several key factors that healthcare providers must consider:
- Data Compatibility: Different wearable devices generate data in various formats. Ensuring that this data can be easily integrated into electronic health records (EHRs) is crucial for effective use.
- Interoperability: Health systems must establish standards that allow different devices and software to communicate with one another. This interoperability is essential for creating a cohesive healthcare experience.
- Patient Engagement: For integration to be successful, patients must be willing to use these devices and share their data. This requires education and encouragement from healthcare providers.
Despite these challenges, the benefits of integration are substantial. For instance, wearable devices can provide continuous monitoring of chronic conditions like diabetes or heart disease. This data can alert healthcare providers to potential issues before they become serious, allowing for timely interventions. Moreover, patients equipped with wearables often feel more empowered and engaged in their own health management, leading to better health outcomes.
To illustrate the impact of this integration, let’s take a look at a hypothetical scenario:
| Wearable Device | Data Collected | Healthcare Provider Action |
|---|---|---|
| Smartwatch | Heart rate, activity levels | Adjust medication based on activity data |
| Glucose Monitor | Blood sugar levels | Send alerts for abnormal readings |
| Fitness Tracker | Sleep patterns, exercise | Recommend lifestyle changes |
This table showcases how different wearables can provide critical data that informs healthcare provider decisions, leading to a more proactive approach to patient care. The integration of health systems with wearable technology not only enhances patient monitoring but also fosters a collaborative relationship between patients and healthcare providers.
In conclusion, as wearable health technology continues to evolve, its integration with health systems will be vital in shaping the future of healthcare. By addressing the challenges of data compatibility, interoperability, and patient engagement, we can unlock the full potential of these devices to improve health outcomes and enhance the overall patient experience.
Q: What types of wearable devices can be integrated into health systems?
A: Wearable devices such as smartwatches, fitness trackers, and specialized medical monitors can all be integrated into health systems to provide valuable health data.
Q: How does data from wearables improve patient care?
A: Data from wearables allows healthcare providers to monitor patients' health in real-time, enabling timely interventions and personalized treatment plans.
Q: What are the privacy concerns with wearable technology?
A: Privacy concerns include the security of personal health data and the potential for unauthorized access. It's crucial for health systems to implement robust data protection measures.

Future Trends in Wearables
As we look ahead, the landscape of wearable health technology is poised for a remarkable transformation. The future trends in wearables are not just about making devices smaller or more stylish; they are fundamentally about enhancing how we approach health management. One of the most exciting trends is the integration of artificial intelligence into wearables, which will allow these devices to not only collect data but also analyze it in real-time. Imagine your smartwatch not only tracking your heart rate but also predicting potential health issues before they arise. This is not science fiction; it’s the future of personal health monitoring.
Moreover, the development of biometric sensors is set to revolutionize the wearable market. These sensors can measure a variety of health metrics, from blood glucose levels to hydration status, providing users with a comprehensive view of their health. For instance, a future wearable might integrate multiple sensors to monitor vital signs continuously, sending alerts directly to healthcare providers if any readings fall outside of normal ranges. This proactive approach to health management could drastically reduce emergency situations and enhance overall patient outcomes.
Another key trend is the increased focus on interoperability. As more people adopt wearable devices, the need for these devices to communicate with each other and with healthcare systems becomes crucial. Future wearables will likely feature enhanced connectivity options, allowing seamless data sharing between devices and healthcare providers. This integration will empower patients by providing them with a holistic view of their health data, making it easier to manage chronic conditions or monitor recovery after surgery.
Additionally, we can expect a surge in the use of augmented reality (AR) in wearables. Imagine a pair of smart glasses that not only assist with navigation but also provide real-time health information about your surroundings or even guide you through rehabilitation exercises. This fusion of AR and wearables could create immersive experiences that enhance patient engagement and adherence to treatment plans.
However, with all these advancements come challenges. Data privacy remains a significant concern, especially as wearables collect more sensitive health information. Manufacturers will need to prioritize security features to protect user data from breaches. Furthermore, as wearables become more sophisticated, the potential for regulatory scrutiny increases. Ensuring that these devices meet safety and efficacy standards will be essential for gaining public trust.
In conclusion, the future of wearable technology in healthcare is bright and full of potential. With innovations like AI integration, advanced biometric sensors, improved interoperability, and AR applications, wearables are set to empower individuals to take control of their health like never before. As we embrace these changes, the key will be to balance innovation with ethical considerations, ensuring that technology serves to improve health outcomes while safeguarding personal information.
- What are wearables? Wearables are electronic devices that can be worn on the body, often incorporating sensors to monitor health metrics.
- How do wearables improve health management? They provide real-time data, enabling proactive health monitoring and personalized treatment plans.
- What are the privacy concerns associated with wearables? The collection of sensitive health data raises issues regarding data security and patient confidentiality.
- Will wearables replace traditional healthcare? No, wearables complement traditional healthcare by enhancing patient engagement and data collection.
Frequently Asked Questions
- What is telemedicine and how has it changed healthcare?
Telemedicine refers to the use of digital technologies to provide healthcare services remotely. It has revolutionized healthcare by allowing patients to consult with medical professionals from the comfort of their homes, reducing travel time and increasing access to care, especially for those in rural areas.
- How does artificial intelligence improve diagnostics?
Artificial intelligence enhances diagnostics by analyzing vast amounts of medical data quickly and accurately. AI tools can assist healthcare providers in detecting diseases earlier and developing personalized treatment plans, ultimately leading to better patient outcomes.
- What are machine learning algorithms and their role in healthcare?
Machine learning algorithms are a subset of AI that can learn from data patterns. In healthcare, they are used to predict patient outcomes, identify risk factors, and tailor treatment plans, making healthcare more proactive rather than reactive.
- What are the data privacy concerns associated with AI in healthcare?
With the integration of AI in healthcare, data privacy concerns arise regarding the security of sensitive patient information. Ethical considerations include ensuring that patient data is protected from breaches and misuse while still allowing for the effective use of AI in treatment and diagnostics.
- What regulatory challenges does AI face in healthcare?
As AI applications in healthcare expand, they encounter regulatory challenges such as the need for clear guidelines and standards to ensure safety and efficacy. Regulatory bodies must keep pace with technological advancements to protect patients while fostering innovation.
- How does telehealth improve healthcare accessibility?
Telehealth significantly improves healthcare accessibility by providing services to individuals in remote or underserved areas. It bridges gaps in care, allowing patients to receive timely medical attention without the barriers of distance or transportation.
- What advancements are being made in wearable health technology?
Wearable health technology has seen significant advancements, including more accurate sensors and integration with mobile apps. These devices allow patients to monitor vital signs and health metrics in real-time, empowering them to take charge of their health.
- How can wearable technology be integrated with existing health systems?
Integrating wearable technology with existing health systems can enhance data collection and patient management. However, challenges include ensuring compatibility with current systems and addressing data privacy concerns, which require careful planning and execution.
- What are the future trends in wearable health technology?
The future of wearable health technology is promising, with trends such as advanced biometric sensors and AI-driven health insights. These innovations aim to provide patients with even more tools for managing their health and improving preventive care.