The Biology of Immune Function - Staying Healthy
Welcome to the fascinating world of the immune system! It's not just a collection of cells and proteins; it's a complex, dynamic network that works tirelessly to protect your body from a myriad of threats. Think of your immune system as a highly skilled army, always on alert, ready to defend your health against invading pathogens like bacteria, viruses, and even some types of cancer cells. Its primary mission? To maintain homeostasis—that delicate balance that keeps you feeling your best.
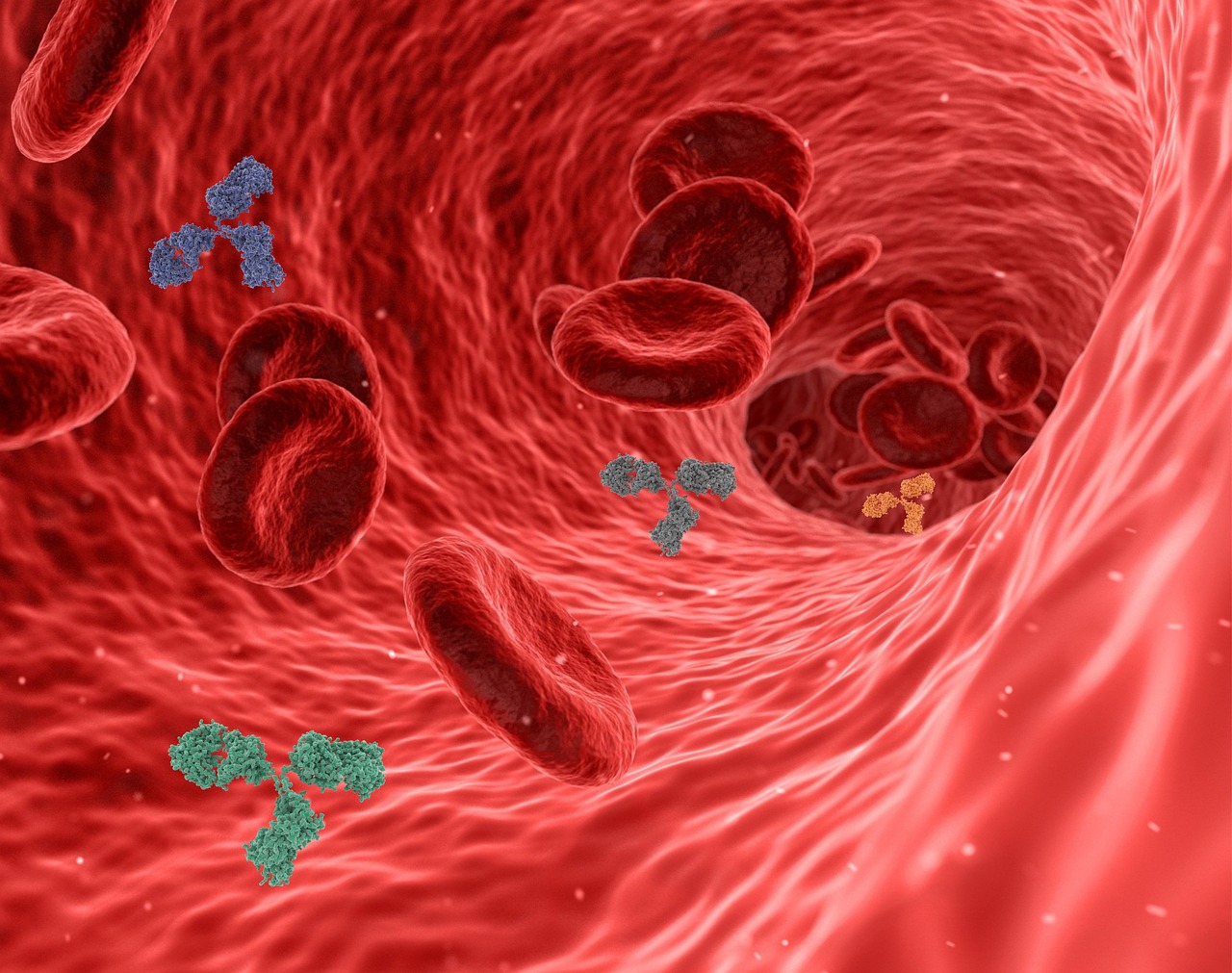
The immune system is comprised of various components, including white blood cells, antibodies, and specialized organs like the spleen and thymus. Together, they form an intricate defense mechanism that not only identifies and neutralizes harmful invaders but also remembers them for future encounters. This ability to remember is what sets the immune system apart; it evolves and adapts, ensuring that subsequent exposures to the same pathogens are met with a swift and effective response.
But how does this all work? Imagine your immune system like a well-coordinated orchestra. Each section—strings, brass, woodwinds—represents different components of the immune response, working together to create a harmonious defense. When a pathogen breaches your body's defenses, the immune system springs into action, mobilizing various cells and signaling molecules to tackle the threat. This response can be immediate, as seen in innate immunity, or more refined and targeted, as observed in adaptive immunity.
In this article, we will delve deeper into the different types of immunity, the disorders that can affect this vital system, and how you can support your immune health through nutrition and lifestyle choices. After all, staying healthy is not just about avoiding illness; it's about understanding and nurturing the incredible biological processes that keep your body functioning optimally.
The immune system operates as the body’s defense mechanism against harmful intruders. It consists of two main types of immunity: innate and adaptive. Innate immunity is your first line of defense, acting quickly and non-specifically to eliminate threats. On the other hand, adaptive immunity takes a bit longer to kick in but provides a targeted response that can remember specific pathogens for future encounters.
Each component of the immune system plays a unique role. For instance, phagocytes are like the foot soldiers, engulfing and destroying pathogens, while B and T cells are the strategists, coordinating the response and remembering past invaders. This intricate dance of cells and proteins is what keeps you healthy and ready to face the world.
Understanding the types of immunity is crucial for grasping how our bodies defend themselves. Let's break it down:
Innate immunity is the body’s immediate response to pathogens. It includes physical barriers like skin and mucous membranes, which act as the first line of defense. If an invader breaches these barriers, the innate immune system deploys various immune cells to neutralize the threat.
Your skin is like a fortress, shielding your body from harmful invaders. Mucous membranes lining your respiratory and digestive tracts also play a crucial role in trapping pathogens. These barriers are essential for maintaining your overall health and preventing infections.
Within the innate immune system, cells like phagocytes and natural killer cells act rapidly to eliminate pathogens. Phagocytes engulf and digest invaders, while natural killer cells target and destroy infected or cancerous cells. This swift response is vital for controlling infections before they escalate.
Adaptive immunity develops over time and is characterized by its ability to remember specific pathogens. This is achieved through memory cells that remain in the body long after an infection has cleared, allowing for a faster and more effective response upon re-exposure.
While our immune system is incredibly efficient, it can sometimes malfunction, leading to disorders such as autoimmune diseases and immunodeficiencies. These conditions can have significant implications for health and well-being.
Autoimmune diseases occur when the immune system mistakenly attacks healthy cells, mistaking them for foreign invaders. This miscommunication can lead to a range of health complications, requiring careful management and treatment.
Immunodeficiencies result in a weakened immune response, making individuals more susceptible to infections. These conditions can be congenital or acquired, often requiring medical intervention to help prevent and treat infections effectively.
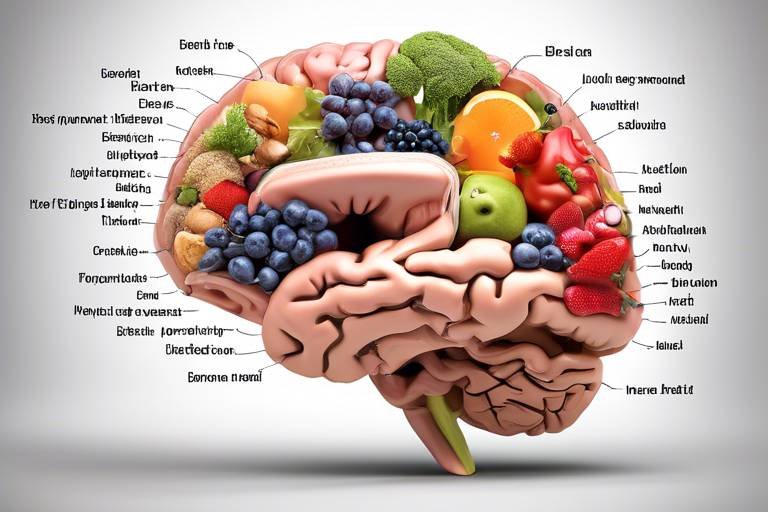
What you eat can significantly impact your immune function. A balanced diet rich in essential nutrients supports your immune system and promotes overall health. Vitamins and minerals play vital roles in enhancing immune responses and maintaining optimal function.
Certain vitamins and minerals, such as vitamin C, vitamin D, and zinc, are crucial for a robust immune response. Incorporating these nutrients into your diet can help bolster your body's defenses against pathogens.
Staying hydrated is equally important. Proper hydration supports various bodily functions, including the immune system's ability to respond effectively to threats. Aim to drink plenty of water throughout the day to keep your body functioning at its best.
Your lifestyle choices can also influence your immune health. Regular exercise, adequate sleep, and effective stress management are all key components of a robust immune system.
Engaging in regular physical activity boosts immune function by enhancing circulation and promoting overall health. Think of exercise as a natural way to invigorate your immune system and keep it resilient against infections.
Don't underestimate the power of sleep! Adequate rest allows your body to repair and regenerate, ensuring optimal immune responses. Prioritizing sleep is essential for keeping your immune system in top shape.
Vaccination is a crucial tool in preventing infectious diseases. By stimulating the immune system to recognize and combat specific pathogens, vaccines enhance your body’s ability to fend off infections.
There are different types of vaccines, including live-attenuated, inactivated, and mRNA vaccines. Each type works by training your immune system to develop memory against specific pathogens, providing long-term protection.
Understanding vaccine efficacy and safety is vital for informed decision-making. Vaccines play a significant role in public health, protecting not only individuals but also communities by reducing the spread of infectious diseases.
- What is the immune system? The immune system is a complex network of cells and proteins that defends the body against harmful invaders.
- How can I boost my immune system? You can boost your immune system through a balanced diet, regular exercise, adequate sleep, and proper hydration.
- What are autoimmune diseases? Autoimmune diseases occur when the immune system mistakenly attacks healthy cells, leading to various health complications.
- Why are vaccines important? Vaccines are important because they train the immune system to recognize and combat specific pathogens, preventing infections.

The Immune System Overview
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful invaders such as bacteria, viruses, and parasites. Think of it as your body's very own security team, constantly on the lookout for potential threats. This intricate system plays a crucial role not only in protecting you from disease but also in maintaining overall homeostasis, ensuring that everything in your body functions optimally.
At its core, the immune system comprises various components, including white blood cells, antibodies, and the lymphatic system. White blood cells, or leukocytes, are the soldiers of the immune system, ready to spring into action at the first sign of danger. They are produced in the bone marrow and can be found circulating in your bloodstream, patrolling for intruders. Antibodies, on the other hand, are specialized proteins created by the immune system to identify and neutralize pathogens.
The lymphatic system, which includes lymph nodes and vessels, acts as a highway for immune cells, transporting them to where they are needed most. When an infection occurs, lymph nodes can swell as they produce more immune cells to combat the threat. This response is a clear indication that your immune system is hard at work, often manifesting as the swelling or tenderness you might feel in your neck or underarms when you're sick.
One of the most fascinating aspects of the immune system is its ability to "remember" past infections. This is where the concept of immunity comes into play. After an initial exposure to a pathogen, the immune system creates memory cells that allow it to respond more swiftly and effectively if the same pathogen tries to invade again. This is the principle behind vaccinations, which prepare your immune system to recognize and fight specific diseases without causing the illness itself.
In summary, the immune system is not just a collection of cells and organs; it is a dynamic and responsive network that plays an essential role in your health. By understanding how it works, you can take proactive steps to support your immune function, ensuring that your body remains resilient against the myriad of threats it faces daily.

The immune system is a complex network that plays a vital role in defending our bodies against harmful pathogens. Understanding the types of immunity is essential for grasping how our bodies fight off infections and maintain health. There are two primary types of immunity: innate immunity and adaptive immunity. Each of these types has unique characteristics and functions, working together to ensure our bodies can effectively respond to various threats.
Innate immunity is the body's first line of defense. Imagine it as the vigilant guard at the entrance of a castle, always on the lookout for intruders. This type of immunity is present from birth and responds quickly to pathogens without needing previous exposure. It includes various physical barriers, like skin and mucous membranes, as well as immune cells that act swiftly to eliminate invaders. The innate immune response is rapid and non-specific, meaning it doesn't target specific pathogens but rather provides a general defense against anything deemed a threat.
On the other hand, adaptive immunity is more like a specialized military unit that develops over time. This type of immunity kicks in after the innate response and is tailored to recognize and remember specific pathogens. Once the body encounters a pathogen, it creates memory cells that "remember" how to fight it off in the future. This is why, for instance, after recovering from chickenpox, you're less likely to get it again. Adaptive immunity is slower to respond initially but provides a targeted and long-lasting defense against specific invaders.
Both types of immunity are crucial for maintaining health. While innate immunity provides immediate defense, adaptive immunity offers a more refined and lasting protection. Together, they create a robust immune system capable of responding to a wide range of infections. Understanding these two types can empower individuals to make informed health choices, such as getting vaccinated or maintaining a healthy lifestyle to support their immune function.
In summary, the interplay between innate and adaptive immunity is fundamental to our overall health. By recognizing how these systems function, we can better appreciate the importance of our immune system and the ways we can support it through lifestyle choices, nutrition, and preventive measures.
- What is the main difference between innate and adaptive immunity?
Innate immunity is the body's immediate, non-specific response to pathogens, while adaptive immunity develops over time and provides a targeted response to specific invaders. - How does vaccination relate to adaptive immunity?
Vaccination exposes the immune system to a harmless part of a pathogen, allowing the body to develop memory cells that provide long-term protection against future infections. - Can lifestyle choices affect my immune system?
Absolutely! Factors like nutrition, exercise, and sleep can significantly influence the effectiveness of both innate and adaptive immunity.

When it comes to defending our bodies against invading pathogens, innate immunity is like the first responders at the scene of an emergency. This type of immunity is our body's initial line of defense, acting swiftly and effectively to thwart the entry of harmful microbes. Unlike its counterpart, adaptive immunity, which takes time to develop a targeted response, innate immunity is always ready to spring into action without needing prior exposure to a pathogen. Think of it as a security system that is always on alert, ready to sound the alarm at the first sign of trouble.
One of the key features of innate immunity is its physical barriers, which include our skin and mucous membranes. These barriers serve as the frontline troops, blocking pathogens from entering the body in the first place. The skin, for instance, is not just a protective covering; it also produces antimicrobial substances that help to neutralize potential threats. Mucous membranes, found in areas such as the respiratory and digestive tracts, trap pathogens and contain enzymes that can break them down. It's like having a fortress with moats and walls, making it difficult for invaders to breach our defenses.
In addition to these physical barriers, innate immunity relies on a variety of cellular defenses to combat infections. Immune cells, such as phagocytes and natural killer (NK) cells, play a crucial role in this process. Phagocytes, like macrophages, are the body's scavengers; they engulf and digest harmful particles, including bacteria and dead cells. Meanwhile, NK cells patrol the body, identifying and destroying infected or cancerous cells. These cellular defenders act quickly, often within hours of an infection, showcasing the rapid response capabilities of the innate immune system.
To summarize, innate immunity is an essential aspect of our overall health, acting as a first line of defense against diseases. Its combination of physical barriers and cellular responses ensures that our bodies are equipped to handle a wide range of pathogens, often before we even realize an infection has occurred. This system not only protects us but also lays the groundwork for the more specialized responses of adaptive immunity, creating a comprehensive defense strategy that keeps us healthy and resilient.
- What is the difference between innate and adaptive immunity? Innate immunity is the body's immediate response to pathogens, while adaptive immunity develops over time and targets specific invaders.
- How do physical barriers contribute to innate immunity? Physical barriers like skin and mucous membranes prevent pathogens from entering the body, acting as the first line of defense.
- What role do immune cells play in innate immunity? Immune cells such as phagocytes and natural killer cells quickly respond to infections by engulfing pathogens and destroying infected cells.

The first line of defense in our body’s intricate immune system is made up of physical barriers. Think of these barriers as the walls of a fortress, designed to keep out invaders. The most prominent of these barriers is our skin, which acts as a tough shield against a multitude of pathogens. Just like a sturdy gate, our skin prevents bacteria, viruses, and other harmful microorganisms from entering the body. But it doesn’t stop there; our body has additional layers of protection that work tirelessly to maintain health and well-being.
Another crucial component of our physical defenses is the mucous membranes, which line various cavities and organs. These membranes produce mucus, a sticky substance that traps pathogens and prevents them from penetrating deeper into the body. Imagine these membranes as a net that catches fish; they ensnare harmful invaders before they can cause harm. In addition, the mucus contains antibodies and enzymes that further aid in neutralizing threats.
Moreover, our body employs various other physical barriers, such as:
- Hair and Cilia: Found in the respiratory tract, hair and tiny hair-like structures called cilia help trap dust and pathogens, pushing them out of the body. This is similar to a broom sweeping away dirt.
- Saliva: The mouth produces saliva, which contains enzymes that break down pathogens. This is akin to having a built-in cleaning solution that helps keep our oral cavity safe.
- Stomach Acid: The highly acidic environment in our stomach acts as a barrier, killing many pathogens ingested with food. It's like a boiling cauldron that destroys anything harmful that slips through.
These physical barriers not only provide immediate protection but also play a vital role in the overall immune response. When these barriers are compromised, such as through cuts or abrasions, pathogens can invade more easily, leading to infections. Therefore, maintaining the integrity of these barriers is essential. This can be achieved through proper hygiene, a balanced diet, and adequate hydration, all of which contribute to the health of our skin and mucous membranes.
In conclusion, physical barriers are the unsung heroes of our immune system. They work silently but effectively to keep us safe from a world teeming with potential threats. By understanding and appreciating these defenses, we can take proactive steps to support them, ensuring that our immune system remains robust and ready to fight off any invaders.
- What are physical barriers in the immune system?
Physical barriers include the skin, mucous membranes, and other protective surfaces that prevent pathogens from entering the body. - How do physical barriers protect against infections?
They act as the first line of defense, trapping and neutralizing harmful microorganisms before they can cause harm. - Can physical barriers be compromised?
Yes, cuts, abrasions, or poor hygiene can weaken these barriers, making it easier for pathogens to invade. - How can I support my physical barriers?
Maintaining good hygiene, eating a balanced diet, and staying hydrated are key ways to support your body's physical barriers.

This article explores the intricate mechanisms of the immune system, its various components, and how they work together to protect the body against diseases, ultimately contributing to overall health and well-being.
An introduction to the immune system, discussing its primary functions, components, and the essential role it plays in defending the body against pathogens and maintaining homeostasis.
This section covers the two main types of immunity: innate and adaptive, explaining their differences, how they function, and their significance in the immune response.
Innate immunity serves as the body's first line of defense, utilizing physical barriers and immune cells to respond quickly to pathogens without prior exposure.
Physical barriers such as skin and mucous membranes play a crucial role in preventing pathogen entry and maintaining the body's overall health.
When it comes to defending our bodies against invaders, cellular defenses are like the elite soldiers of our immune army. These specialized cells are always on high alert, ready to spring into action at a moment's notice. Among these defenders, we find phagocytes and natural killer (NK) cells. Phagocytes, such as macrophages and neutrophils, are like the vacuum cleaners of the immune system. They roam around, identifying and engulfing pathogens, effectively eliminating them from the body. Imagine them as diligent janitors, constantly cleaning up the mess left by harmful microbes.
Natural killer cells, on the other hand, are the assassins of the immune system. They target and destroy infected or cancerous cells without needing prior exposure to the threat. This ability to recognize and eliminate compromised cells makes them crucial in the early stages of an infection. Think of them as the secret agents who can infiltrate enemy lines and take down threats before they can cause significant harm.
In addition to these two main types of cells, the innate immune system also employs a variety of signaling molecules and proteins, such as cytokines and complement proteins, to coordinate the immune response. Cytokines act like messengers, communicating with other immune cells to amplify the response and ensure a swift reaction. Complement proteins enhance the ability of antibodies and phagocytic cells to clear pathogens from an organism. Together, these cellular defenses create a robust and dynamic response to any potential threat, ensuring that our body remains a fortress against disease.
This section examines various disorders affecting the immune system, including autoimmune diseases and immunodeficiencies, highlighting their causes and implications for health.
Autoimmune diseases occur when the immune system mistakenly attacks healthy cells, leading to various health complications and requiring careful management.
Immunodeficiencies result in a weakened immune response, making individuals more susceptible to infections and diseases, often requiring medical intervention for prevention and treatment.
Exploring the impact of nutrition on immune function, this section emphasizes the importance of a balanced diet in supporting the immune system and promoting overall health.
Certain vitamins and minerals, such as vitamin C, D, and zinc, play vital roles in enhancing immune responses and maintaining optimal immune function.
Staying hydrated is crucial for overall health, as proper hydration supports various bodily functions, including the immune system's ability to respond effectively to pathogens.
This section discusses how lifestyle choices, such as exercise, sleep, and stress management, influence immune health and contribute to a robust immune system.
Regular physical activity has been shown to boost immune function, enhance circulation, and promote overall health, making it a key factor in maintaining immune resilience.
Adequate sleep is essential for a healthy immune system, as it allows the body to repair and regenerate, ensuring optimal immune responses to infections.
Vaccination is a crucial tool in preventing infectious diseases, enhancing the immune system's ability to recognize and combat specific pathogens effectively.
Different types of vaccines, including live-attenuated, inactivated, and mRNA vaccines, work by stimulating the immune system to develop memory against specific pathogens.
Understanding vaccine efficacy and safety is vital for informed decision-making, as vaccines play a significant role in public health and individual immunity.
Q: What is the role of phagocytes in the immune system?
A: Phagocytes, such as macrophages and neutrophils, engulf and destroy pathogens, acting as the body's cleanup crew.
Q: How do natural killer cells differ from other immune cells?
A: Natural killer cells can recognize and eliminate infected or cancerous cells without prior exposure, making them vital for early immune responses.
Q: What dietary changes can support immune health?
A: A balanced diet rich in vitamins and minerals, particularly vitamin C, D, and zinc, can enhance immune function.
Q: How does exercise affect the immune system?
A: Regular physical activity boosts immune function and circulation, contributing to overall health and resilience against infections.

Adaptive immunity is like a well-trained army that gets stronger with every battle it faces. Unlike innate immunity, which is the body's first line of defense, adaptive immunity takes time to develop but provides a highly specific response to pathogens. When your body encounters a virus or bacteria for the first time, it goes through a process of recognizing and remembering that invader. This memory is what makes adaptive immunity so powerful—it allows your immune system to respond more effectively and rapidly upon subsequent exposures to the same pathogen.
The adaptive immune response primarily involves two types of cells: B cells and T cells. B cells are responsible for producing antibodies, which are proteins that can specifically bind to pathogens and neutralize them. Imagine antibodies as tiny locks that fit perfectly into the keys (pathogens) trying to invade your body. Once they bind, they can either block the pathogen from entering your cells or mark it for destruction by other immune cells.
On the other hand, T cells come in different varieties, each with a unique role. Helper T cells assist B cells in producing antibodies, while killer T cells seek out and destroy infected cells. This teamwork is essential for a robust immune response. The beauty of adaptive immunity lies in its ability to remember past infections. Once B and T cells encounter a pathogen, they create memory cells that linger long after the infection has cleared. This means that if the same pathogen tries to invade again, your immune system is already prepared, leading to a quicker and more efficient response.
In addition to the cellular components, the adaptive immune system also relies on a complex network of signaling molecules called cytokines. These molecules act like messengers, coordinating the activities of various immune cells and ensuring that the response is well-organized. The entire process is a fine-tuned symphony, where each player has a role to ensure that the body remains healthy and free from disease.
However, adaptive immunity is not just about fighting infections; it also plays a crucial role in the effectiveness of vaccines. Vaccines work by introducing a harmless part of a pathogen (like a piece of its protein) into the body, prompting the adaptive immune system to respond as if it were facing an actual infection. This leads to the formation of memory cells without the person suffering from the disease. Thus, when exposed to the real pathogen later on, the immune system can mount a swift and effective response, often preventing illness altogether.
In summary, adaptive immunity is a sophisticated defense mechanism that enhances the body's ability to fight infections through memory, specificity, and coordination. It is a remarkable example of how our bodies can learn and adapt, ensuring that we are better equipped to handle the challenges posed by various pathogens in our environment.
- What is the difference between innate and adaptive immunity? Innate immunity is the first line of defense and responds quickly to pathogens, while adaptive immunity takes longer to develop but provides a targeted and memory-based response.
- How do vaccines work in relation to adaptive immunity? Vaccines stimulate the adaptive immune system to create memory cells that recognize specific pathogens, allowing for a faster and more effective response upon future exposure.
- Can adaptive immunity be improved? Yes, maintaining a healthy lifestyle, including proper nutrition, regular exercise, and adequate sleep, can enhance the effectiveness of the adaptive immune system.

The immune system is a complex network of cells and proteins that defends the body against infections and diseases. However, when this intricate system goes awry, it can lead to various disorders that significantly impact health. Understanding these disorders is crucial for recognizing symptoms and seeking appropriate treatment. Immune system disorders can be broadly classified into two categories: autoimmune diseases and immunodeficiencies. Each of these conditions has distinct causes and implications for overall health.
Autoimmune diseases occur when the immune system mistakenly identifies healthy cells as foreign invaders, launching an attack that can lead to inflammation and damage. This misdirected immune response can affect various organs and systems in the body, resulting in a wide range of symptoms. Common autoimmune diseases include rheumatoid arthritis, lupus, and multiple sclerosis. The exact cause of autoimmune diseases remains unclear, but it is believed that a combination of genetic predisposition, environmental triggers, and infections may play a role. Living with an autoimmune disease often requires careful management, including medications to suppress the immune response and lifestyle adjustments to alleviate symptoms.
On the other hand, immunodeficiencies occur when the immune system is weakened or dysfunctional, leaving the body vulnerable to infections and diseases. These conditions can be either primary (genetic) or secondary (acquired), with primary immunodeficiencies being rare and often diagnosed in childhood. Secondary immunodeficiencies can arise from factors such as malnutrition, certain medications, or infections like HIV/AIDS. Individuals with immunodeficiencies may experience frequent infections, prolonged illness, and complications that can significantly affect their quality of life. Treatment typically involves managing infections, boosting the immune response, and in some cases, immunoglobulin therapy or stem cell transplants.
To better understand the differences between autoimmune diseases and immunodeficiencies, consider the following table:
| Type of Disorder | Description | Examples |
|---|---|---|
| Autoimmune Diseases | The immune system attacks healthy cells, mistaking them for pathogens. | Rheumatoid arthritis, lupus, multiple sclerosis |
| Immunodeficiencies | The immune system is weakened, leading to increased susceptibility to infections. | HIV/AIDS, congenital immunodeficiency disorders |
Recognizing the signs and symptoms of these disorders is essential for early intervention and effective management. If you or someone you know is experiencing unexplained fatigue, recurrent infections, or chronic inflammation, it may be worth consulting a healthcare professional for further evaluation. Knowledge is power, and understanding the intricacies of immune system disorders can pave the way for better health outcomes.
- What are the common symptoms of autoimmune diseases? Symptoms can vary widely but often include fatigue, joint pain, skin rashes, and fever.
- How are immunodeficiencies diagnosed? Diagnosis typically involves blood tests to assess immune function and identify specific deficiencies.
- Can lifestyle changes help manage immune system disorders? Yes, a balanced diet, regular exercise, and stress management can positively impact immune health.

Autoimmune diseases are a fascinating yet complex area of health that arise when the body's own immune system, which is designed to protect us from harmful invaders, mistakenly targets and attacks healthy cells. Imagine your immune system as a highly trained army that, instead of defending the fortress, starts firing upon its own soldiers. This misdirected attack can lead to a variety of health complications, depending on which tissues and organs are affected.
There are over 80 different types of autoimmune diseases, each with its own unique symptoms and challenges. Some of the most well-known include rheumatoid arthritis, lupus, multiple sclerosis, and type 1 diabetes. These conditions can be debilitating, leading to chronic pain, fatigue, and a host of other symptoms that can significantly impact a person's quality of life. The causes of autoimmune diseases are still not fully understood, but they are believed to result from a combination of genetic predisposition, environmental factors, and possibly infections that trigger the immune response.
One of the most perplexing aspects of autoimmune diseases is their unpredictable nature. Symptoms can fluctuate, with periods of exacerbation followed by times of remission. This variability can make diagnosis and treatment difficult. For instance, someone with lupus might experience a flare-up of symptoms after exposure to sunlight or stress, while others may find that certain foods exacerbate their condition. This inconsistency can feel like a rollercoaster ride, leaving patients and healthcare providers alike scrambling for effective management strategies.
The diagnosis of autoimmune diseases often involves a combination of medical history, physical examinations, and laboratory tests. Blood tests can reveal the presence of specific autoantibodies, which are markers that indicate an autoimmune response. However, the absence of these markers does not rule out the possibility of an autoimmune disease, showcasing the complexity of these conditions.
Management of autoimmune diseases typically requires a multifaceted approach. This may include:
- Medications: Anti-inflammatory drugs, immunosuppressants, and corticosteroids are commonly prescribed to reduce inflammation and suppress the overactive immune response.
- Lifestyle Modifications: Diet and exercise play crucial roles in managing symptoms. Many patients find that certain dietary changes, such as reducing processed foods or increasing omega-3 fatty acids, can help alleviate symptoms.
- Regular Monitoring: Ongoing communication with healthcare providers is essential to adjust treatment plans as needed and to monitor for any potential complications.
Living with an autoimmune disease can be challenging, but support systems, whether through family, friends, or support groups, can make a significant difference. Understanding the condition, advocating for oneself, and seeking professional guidance are key components in navigating this complex landscape. As research continues to evolve, hope remains that more effective treatments and possibly even cures will emerge, providing relief and improved quality of life for those affected.
Q: What are the common symptoms of autoimmune diseases?
A: Symptoms vary widely but may include fatigue, joint pain, skin rashes, and fever. Each autoimmune disease has its own specific symptoms.
Q: Are autoimmune diseases hereditary?
A: Genetics can play a role in the likelihood of developing an autoimmune disease, but environmental factors and lifestyle choices are also significant contributors.
Q: Can autoimmune diseases be cured?
A: Currently, there is no cure for autoimmune diseases, but many can be managed effectively with medication and lifestyle changes.
Q: How can I support someone with an autoimmune disease?
A: Providing emotional support, helping with daily tasks, and encouraging them to seek medical advice can be invaluable to someone battling an autoimmune condition.

Immunodeficiencies represent a critical challenge to the immune system's ability to function effectively. When we think about our immune system, we often picture a robust defense mechanism, ready to fight off infections and diseases. However, for some individuals, this defense is compromised. Immunodeficiencies can be classified into two main categories: primary and secondary. Primary immunodeficiencies are often genetic, resulting from inherited disorders that affect the immune system's development or function. In contrast, secondary immunodeficiencies are acquired due to external factors such as infections, malnutrition, or certain medical treatments.
The implications of immunodeficiencies can be profound. Individuals with these conditions may experience frequent infections, which can range from mild to life-threatening. For instance, a common cold could escalate into pneumonia, simply because the body lacks the necessary defenses to combat it. This vulnerability can lead to a cycle of illness that not only affects physical health but can also take a toll on mental well-being. Imagine feeling constantly on edge, worried about the next bout of illness; it’s an exhausting reality for many.
One of the most well-known examples of a primary immunodeficiency is Severe Combined Immunodeficiency (SCID), often referred to as "bubble boy disease." Infants born with SCID have a severely weakened immune system and must live in sterile environments to avoid infections. Without treatment, which often involves bone marrow transplants or gene therapy, these children may not survive beyond their first year. This highlights the importance of early diagnosis and intervention.
On the other hand, secondary immunodeficiencies can arise from various conditions. For example, individuals with HIV/AIDS experience a gradual decline in immune function as the virus attacks CD4 T-cells, which are crucial for orchestrating the immune response. Other factors contributing to secondary immunodeficiencies include:
- Chronic diseases such as diabetes or cancer
- Medications like corticosteroids or chemotherapy
- Malnutrition, particularly a lack of essential nutrients
Understanding the causes and effects of immunodeficiencies is vital for effective management and treatment. Healthcare providers often employ a range of strategies to support individuals with these conditions, including vaccinations, prophylactic antibiotics, and lifestyle modifications to boost overall health. Regular check-ups and monitoring are essential to catch potential infections early and to adjust treatments as necessary.
In conclusion, immunodeficiencies pose significant challenges to maintaining health and well-being. By raising awareness and understanding the complexities of these conditions, we can foster a more supportive environment for those affected. As we continue to learn about the immune system, it’s crucial to remember that knowledge is power, and empowering individuals with information can lead to better health outcomes.
- What are the symptoms of immunodeficiencies? Symptoms may include frequent infections, delayed recovery from illnesses, and unexplained weight loss.
- How are immunodeficiencies diagnosed? Diagnosis typically involves blood tests to assess immune function and genetic testing for primary immunodeficiencies.
- Can immunodeficiencies be treated? Treatment options vary depending on the type and severity but may include medications, immunoglobulin therapy, or bone marrow transplants.
When it comes to staying healthy, nutrition plays a pivotal role in supporting our immune system. Imagine your body as a complex fortress, constantly under siege by various pathogens. Just like a fortress needs strong walls and a well-fed army to defend itself, your immune system requires the right nutrients to function optimally. A balanced diet rich in vitamins, minerals, and other essential nutrients can significantly bolster your body’s defenses against infections and diseases.
One of the most critical aspects of nutrition is ensuring that you consume a variety of foods that provide the essential nutrients your immune system craves. For instance, vitamin C is renowned for its immune-boosting properties, found abundantly in citrus fruits, strawberries, and bell peppers. This vitamin helps stimulate the production of white blood cells, which are crucial for fighting off infections. Similarly, vitamin D plays a vital role in immune function, and sources like fatty fish, fortified dairy products, and sunlight exposure can help maintain adequate levels in your body.
Another key player in immune health is zinc. This mineral is essential for the development and function of immune cells. Foods rich in zinc, such as meat, shellfish, legumes, and seeds, can help keep your immune system in top shape. Furthermore, antioxidants found in fruits and vegetables, like vitamin E and beta-carotene, help combat oxidative stress and inflammation, allowing your immune system to operate more efficiently.
Staying hydrated is equally important for immune health. Water is the unsung hero that supports numerous bodily functions, including the transportation of nutrients and the removal of toxins. When you're well-hydrated, your body can effectively produce lymph, which circulates white blood cells and other immune cells throughout your body. Aim to drink plenty of water throughout the day, and consider incorporating hydrating foods like cucumbers, oranges, and watermelon into your diet.
In addition to vitamins and minerals, a healthy gut microbiome is crucial for a robust immune system. The gut houses a significant portion of your immune cells, and a diverse diet rich in fiber, fermented foods, and probiotics can help maintain gut health. Foods like yogurt, kefir, sauerkraut, and whole grains promote the growth of beneficial bacteria, enhancing your body's natural defenses.
In summary, the relationship between nutrition and immune health is undeniable. By prioritizing a well-rounded diet that includes a variety of vitamins, minerals, and hydration, you can empower your immune system to fend off threats effectively. Remember, your body is a fortress, and the food you consume is the armor that protects it. So, what will you choose to nourish your body today?
- How does nutrition affect my immune system?
Nutrition provides the essential nutrients that support immune cell function and overall health, enhancing your body's ability to fight infections. - What foods should I eat to boost my immune system?
Focus on a balanced diet rich in fruits, vegetables, lean proteins, whole grains, and healthy fats, particularly those high in vitamins C, D, and zinc. - Is hydration important for immune health?
Absolutely! Staying hydrated helps maintain bodily functions, including the circulation of immune cells, which is critical for an effective immune response.

When we talk about immune health, we can't overlook the essential roles that vitamins and minerals play in supporting our body's defenses. Think of these nutrients as the building blocks of a strong immune system, working tirelessly behind the scenes to keep us healthy. Just like a well-oiled machine requires the right parts to function smoothly, our immune system needs a variety of vitamins and minerals to operate at its best.
For instance, vitamin C is often hailed as a superhero for immune health. It enhances the function of immune cells and helps them work more efficiently. You can find this powerhouse vitamin in citrus fruits, strawberries, and bell peppers. Similarly, vitamin D plays a critical role in modulating the immune response. A deficiency in vitamin D can lead to increased susceptibility to infections, making it crucial to get enough of this vitamin through sunlight exposure, fatty fish, or fortified foods.
Now, let’s not forget about zinc, a mineral that is equally vital. It is involved in the development and function of immune cells, and a deficiency can severely impair the immune response. Foods rich in zinc include meat, shellfish, legumes, and seeds. To illustrate the importance of these nutrients, consider the following table:
| Nutrient | Role in Immune Function | Food Sources |
|---|---|---|
| Vitamin C | Enhances immune cell function | Citrus fruits, strawberries, bell peppers |
| Vitamin D | Modulates immune response | Sunlight, fatty fish, fortified foods |
| Zinc | Supports immune cell development | Meat, shellfish, legumes, seeds |
In addition to these key players, other vitamins and minerals such as vitamin A and selenium also contribute significantly to maintaining a robust immune system. Vitamin A helps maintain the health of mucosal surfaces, which serve as barriers against pathogens. Selenium, on the other hand, has antioxidant properties that help protect immune cells from damage.
Ultimately, achieving a balanced diet rich in these nutrients is essential for keeping our immune system in top shape. It's not just about taking supplements; it's about nourishing our bodies with whole foods that provide a spectrum of vitamins and minerals. So, next time you sit down for a meal, think about how you're fueling your immune system. Are you including a variety of colorful fruits and vegetables? Are you getting enough healthy fats and proteins? These small choices can make a big difference in your overall health and well-being.
- What are the best food sources for immune-boosting vitamins? Foods like citrus fruits, leafy greens, nuts, and seeds are great sources of vitamins and minerals that support immune health.
- Can I get enough vitamins from supplements? While supplements can help, it's best to obtain vitamins and minerals from a balanced diet to ensure you're getting all the necessary nutrients.
- How does hydration affect immune function? Staying hydrated helps your body function properly, including the immune system, making it easier for your body to fight off infections.

When it comes to maintaining a robust immune system, hydration is often overlooked, yet it plays a critical role in keeping our bodies functioning optimally. Imagine your immune system as a well-oiled machine; without the right amount of fluid, it can start to sputter and slow down. Water is essential for every cell in your body, including those that make up your immune system. It aids in the transport of nutrients, the removal of toxins, and the production of lymph, which is crucial for immune function.
Dehydration can lead to a multitude of issues that can weaken your immune response. For instance, when you're not adequately hydrated, your body struggles to produce enough lymph to circulate white blood cells and other immune components effectively. This can leave you more vulnerable to infections. In fact, studies have shown that even mild dehydration can impair your immune function, making it more difficult for your body to fend off illnesses.
Moreover, staying hydrated supports the mucosal membranes in your respiratory tract. These membranes act as a barrier against pathogens, and when they are dry, they become less effective at trapping and expelling harmful invaders. Think of it like a sponge; when it's dry, it can't absorb anything, but when it's wet, it works perfectly. Similarly, your body's defenses need to be properly hydrated to function at their best.
So, how much water should you be drinking? While the classic advice is to aim for eight 8-ounce glasses a day, individual needs can vary based on factors like age, activity level, and climate. A good rule of thumb is to listen to your body. If you're feeling thirsty, it's a clear sign you need to hydrate. You can also monitor the color of your urine; pale yellow typically indicates proper hydration, while darker shades suggest you need more fluids.
To help you visualize the importance of hydration, here's a simple table that outlines the effects of dehydration on immune function:
| Dehydration Level | Effects on Immune Function |
|---|---|
| Mild Dehydration | Impaired lymph production and reduced white blood cell circulation. |
| Moderate Dehydration | Increased susceptibility to infections and slower recovery times. |
| Severe Dehydration | Significant risk of illness and potential organ failure. |
Incorporating hydration into your daily routine doesn't have to be a chore. You can enhance your fluid intake by consuming water-rich foods such as fruits and vegetables. Foods like cucumbers, oranges, and strawberries can help you stay hydrated while providing essential vitamins and minerals that further support your immune system. Additionally, herbal teas and broths can also contribute to your daily fluid intake.
In conclusion, never underestimate the power of water when it comes to your immune health. Staying hydrated is a simple yet effective strategy to help your body fight off infections and maintain overall well-being. So, next time you reach for a snack, consider a refreshing glass of water or a hydrating fruit instead. Your immune system will thank you!
- How much water should I drink daily? It varies by individual, but a good starting point is about 8 glasses (64 ounces) a day.
- Can I hydrate with beverages other than water? Yes, herbal teas and water-rich foods like fruits and vegetables can also contribute to your hydration.
- What are some signs of dehydration? Thirst, dark urine, fatigue, and dizziness can all indicate that you need more fluids.

When it comes to maintaining a robust immune system, lifestyle factors play a surprisingly vital role. Think of your immune system as a fortress; its strength is not just determined by the walls but also by the resources available within. A balanced lifestyle can enhance your immune defenses, making it crucial to pay attention to various aspects of your daily routine. So, how do we fortify our immune fortress? Let's explore the key lifestyle factors that can help.
First and foremost, exercise is a game-changer. Regular physical activity is like a superhero for your immune system. It boosts circulation, allowing immune cells and antibodies to travel more efficiently throughout your body. Studies have shown that moderate exercise can reduce inflammation and promote the healthy turnover of immune cells. Whether it's a brisk walk, a dance class, or a session at the gym, moving your body regularly can make a significant difference. Just remember, moderation is key; over-exercising can actually have the opposite effect!
Next up is sleep. Imagine trying to build a house without a solid foundation; that’s what it’s like for your immune system without adequate sleep. During sleep, your body undergoes repair and regeneration, producing crucial cytokines that help combat infection and inflammation. If you’re skimping on sleep, you’re not just tired; you’re also compromising your immune response. Aim for 7-9 hours of quality sleep each night to ensure your body has the time it needs to recharge.
Another critical factor is stress management. Chronic stress is like a persistent rainstorm battering your fortress, weakening its defenses over time. When you’re stressed, your body releases hormones like cortisol, which can suppress your immune function. Finding effective ways to manage stress—be it through mindfulness, yoga, or simply taking time to relax—can help keep your immune system strong. Consider incorporating activities that bring you joy, as happiness can boost your immune response!
Nutrition also plays a pivotal role in immunity. A diet rich in whole foods, including fruits, vegetables, whole grains, and lean proteins, provides the essential nutrients your immune system needs to function optimally. Vitamins and minerals such as vitamin C, D, and zinc are particularly important. They act as the building blocks of your immune defenses, helping to produce antibodies and support the function of immune cells. So, think of your plate as your first line of defense; fill it with colorful, nutrient-dense foods!
Lastly, don’t underestimate the power of hydration. Water is essential for every cell in your body, including those that make up your immune system. Staying hydrated helps maintain optimal blood flow, which ensures that immune cells can travel freely to where they’re needed most. Aim to drink enough water throughout the day, and consider incorporating hydrating foods like cucumbers and oranges into your diet.
In summary, lifestyle factors such as exercise, sleep, stress management, nutrition, and hydration are all interconnected elements that contribute to a robust immune system. By making conscious choices in these areas, you can significantly enhance your body's ability to fend off illnesses and maintain overall health. Remember, your immune system is your body's defense mechanism; treat it well, and it will treat you well in return!
- How does exercise boost the immune system? Regular exercise improves circulation, enhances immune cell function, and reduces inflammation.
- What role does sleep play in immunity? Sleep is essential for the production of cytokines and the regeneration of immune cells, which are critical in fighting infections.
- Can stress affect my immune system? Yes, chronic stress can suppress immune function by increasing cortisol levels, making you more susceptible to illness.
- What foods should I eat to support my immune system? A balanced diet rich in fruits, vegetables, whole grains, and lean proteins, particularly those high in vitamins C, D, and zinc, is beneficial.
- How much water should I drink daily? Aim for at least 8 cups (64 ounces) of water a day, but individual needs may vary based on activity and climate.

When it comes to maintaining a robust immune system, exercise is not just a good idea; it's a game changer! Imagine your body as a well-oiled machine, and exercise is the oil that keeps everything running smoothly. Regular physical activity enhances your immune function, making it more efficient at warding off infections and diseases. But how does this happen? Let's dive into the fascinating world of exercise and its impact on our immune response.
Firstly, engaging in moderate exercise increases the circulation of immune cells in the body. Think of these cells as your personal army, ready to defend against any invading pathogens. When you exercise, blood flow increases, which helps these immune cells travel throughout your body more efficiently. This means they can detect and respond to potential threats faster than if you were sedentary. In fact, studies have shown that people who engage in regular moderate exercise experience fewer colds and infections compared to those who lead a sedentary lifestyle.
Moreover, exercise has the added benefit of reducing stress hormones, which can negatively impact your immune system. When you're stressed, your body produces cortisol, a hormone that can suppress immune function. By incorporating physical activity into your routine, you can help mitigate these stress levels, leading to a healthier immune response. It's like giving your immune system a little boost, helping it to operate at peak performance.
However, it's important to strike a balance. While regular exercise is beneficial, excessive or intense workouts can actually have the opposite effect, leading to a temporary decline in immune function. This phenomenon is sometimes referred to as the "open window" theory, where the immune system is compromised for a short period after intense exertion. So, moderation is key! Aim for about 150 minutes of moderate aerobic activity each week, combined with strength training exercises on two or more days.
To help you visualize the benefits of exercise on immune function, here’s a quick table summarizing the key points:
| Benefit | Description |
|---|---|
| Enhanced Circulation | Improves the movement of immune cells throughout the body. |
| Stress Reduction | Decreases cortisol levels, reducing stress on the immune system. |
| Improved Overall Health | Supports weight management and lowers the risk of chronic diseases. |
| Boosted Immune Response | Regular moderate exercise leads to a stronger and more efficient immune system. |
In conclusion, incorporating regular exercise into your lifestyle is one of the best ways to support your immune system. Not only does it enhance circulation and reduce stress, but it also promotes overall well-being. So, whether you prefer running, dancing, or yoga, find an activity you enjoy and make it a part of your routine. Your immune system will thank you!
- How much exercise do I need for optimal immune function? Aim for at least 150 minutes of moderate aerobic activity each week.
- Can too much exercise weaken my immune system? Yes, excessive intense workouts can temporarily lower immune function.
- What types of exercise are best for immune health? A mix of aerobic exercise, strength training, and flexibility activities is ideal.
- How quickly can I see improvements in my immune health from exercise? Many people notice benefits within weeks of starting a regular exercise routine.
When it comes to maintaining a robust immune system, adequate sleep is often an unsung hero. Think of your body as a high-performance vehicle; just like any machine, it needs regular maintenance and proper fuel to run smoothly. Sleep acts as that essential maintenance, allowing your body to repair itself and regenerate vital cells that bolster your immune defenses. During sleep, your body produces cytokines, a type of protein that plays a crucial role in the immune response. These proteins help to combat infections and inflammation, ensuring that your body is ready to tackle any pathogens that may come its way.
But what happens when you skimp on sleep? The consequences can be quite alarming. Research shows that sleep deprivation can lead to a decrease in the production of these protective cytokines, making you more susceptible to illnesses. In fact, a study found that individuals who slept less than seven hours a night were nearly three times more likely to catch a cold compared to those who enjoyed a solid eight hours of shut-eye. It's as if your immune system is throwing in the towel, waving a white flag in surrender when you're not getting enough rest.
Moreover, sleep influences the levels of antibodies and immune cells in your body. These components are essential for identifying and neutralizing harmful invaders. When you’re well-rested, your body can produce more antibodies, which are like the soldiers in your immune army, ready to fight off infections. Conversely, chronic sleep deprivation can lead to a reduction in these critical components, leaving your body vulnerable.
So, how can you ensure you’re getting the quality sleep your immune system craves? Here are a few tips to consider:
- Establish a Sleep Schedule: Go to bed and wake up at the same time every day to regulate your body’s internal clock.
- Create a Relaxing Bedtime Routine: Engage in calming activities such as reading or meditating before bed to signal to your body that it’s time to wind down.
- Limit Screen Time: Reduce exposure to screens at least an hour before bed, as the blue light emitted can interfere with your sleep cycle.
- Optimize Your Sleep Environment: Ensure your bedroom is cool, dark, and quiet to promote restful sleep.
In summary, sleep is not just a luxury; it’s a necessity for a healthy immune system. By prioritizing your sleep, you’re not only giving your body the chance to recharge but also empowering your immune system to function at its best. So, the next time you think about cutting back on sleep to get more done, remember that a well-rested body is a powerful ally in the fight against illness.
- How many hours of sleep do I need for optimal immune function? Generally, adults should aim for 7-9 hours of quality sleep each night to support their immune system.
- Can napping help improve my immune response? Short naps can be beneficial, but they should not replace a full night's sleep. A 20-30 minute nap can help recharge your energy levels.
- What are some signs that my immune system may be weakened? Frequent infections, prolonged wounds healing, and persistent fatigue can indicate a weakened immune system, often linked to inadequate sleep.
- Is there a connection between stress, sleep, and immunity? Yes, chronic stress can disrupt sleep patterns and weaken the immune response, creating a cycle that can be hard to break.
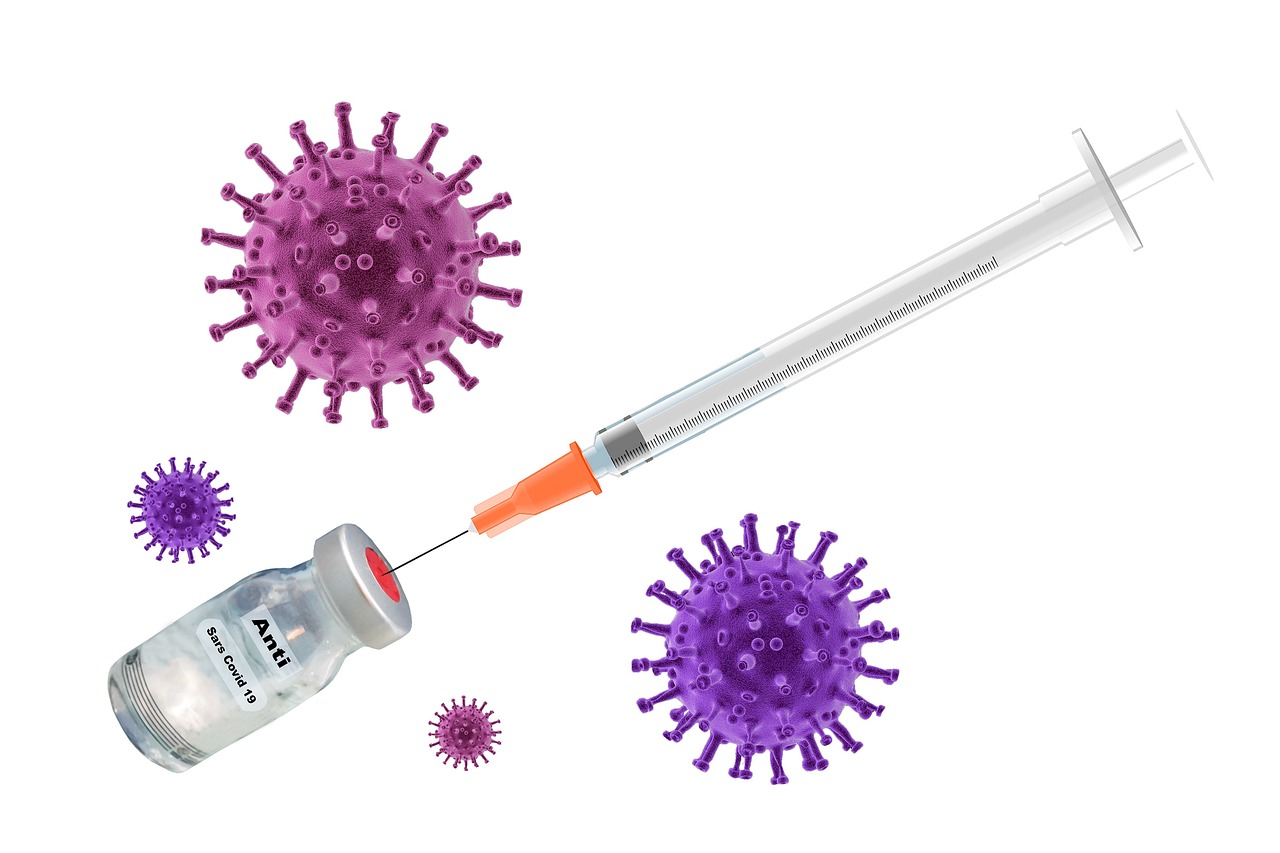
Vaccination is one of the most powerful tools we have in our arsenal to combat infectious diseases. Imagine your immune system as a well-trained army, ready to defend your body against invaders. Vaccines serve as the training ground for this army, teaching it to recognize and fight specific pathogens. By introducing a harmless component of a virus or bacteria—like a piece of its genetic material or a weakened form of the pathogen—vaccines prime your immune system to respond swiftly and effectively when the real threat appears. This process not only protects you but also contributes to the wider community by fostering herd immunity, which is essential for safeguarding those who cannot be vaccinated.
There are several types of vaccines, each designed to stimulate your immune response in different ways. For instance, live-attenuated vaccines contain a weakened form of the virus, while inactivated vaccines use killed pathogens. Then we have mRNA vaccines, which have gained popularity recently due to their role in combating COVID-19. These vaccines work by instructing your cells to produce a harmless piece of the virus, prompting your immune system to kick into gear and prepare for a future encounter with the actual virus.
Understanding vaccine efficacy and safety is crucial for informed decision-making. Vaccines undergo rigorous testing in clinical trials to ensure they are both effective and safe before they are approved for public use. The benefits of vaccination far outweigh the risks, as they significantly reduce the chances of contracting serious illnesses. However, it’s important to stay informed and consult healthcare professionals about the vaccines that are recommended for you and your family, as well as any potential side effects.
Moreover, keeping track of your vaccination schedule is essential. Many vaccines require multiple doses to achieve optimal immunity. For instance, the measles, mumps, and rubella (MMR) vaccine is typically given in two doses, while the HPV vaccine is administered in a series of shots over several months. Staying on top of your vaccinations not only protects you but also helps maintain the health of the community.
| Type of Vaccine | How It Works | Examples |
|---|---|---|
| Live-Attenuated | Contains a weakened form of the germ | MMR, Yellow Fever |
| Inactivated | Contains killed germs | Polio, Hepatitis A |
| mRNA | Teaches cells to make a protein that triggers an immune response | COVID-19 Vaccines (Pfizer, Moderna) |
| Subunit, Recombinant, Polysaccharide, and Conjugate | Includes pieces of the germ (like protein or sugar) to trigger an immune response | HPV, Whooping Cough |
In conclusion, vaccination is a cornerstone of public health that not only protects individuals but also contributes to the well-being of society as a whole. By staying informed and proactive about vaccinations, we can all play a part in preventing the spread of infectious diseases and ensuring a healthier future.
- What are the side effects of vaccines? Most vaccines have mild side effects, such as soreness at the injection site, fatigue, or a low-grade fever.
- Are vaccines safe for everyone? While most people can safely receive vaccines, some individuals may have specific contraindications. It's best to consult with a healthcare provider.
- How do vaccines contribute to herd immunity? When a large portion of the population is vaccinated, it reduces the overall amount of the virus available to spread, protecting those who cannot be vaccinated.
- Do I need to get vaccinated if I've already had the disease? In many cases, vaccination is still recommended even if you've had the disease, as natural immunity may not be sufficient or long-lasting.
Vaccines are a remarkable tool in the fight against infectious diseases, and they come in various types, each designed to elicit a specific immune response. Understanding these types is essential for grasping how vaccines work and their role in public health. The most common categories of vaccines include live-attenuated vaccines, inactivated vaccines, and mRNA vaccines, among others. Each type has its unique characteristics and mechanisms of action, contributing to the overall effectiveness of vaccination programs.
Live-attenuated vaccines contain a weakened form of the virus or bacteria that causes a disease. These vaccines are designed to stimulate a strong immune response without causing the disease itself. For instance, the measles, mumps, and rubella (MMR) vaccine is a classic example. Because they closely mimic a natural infection, live-attenuated vaccines often provide long-lasting immunity with just one or two doses.
On the other hand, inactivated vaccines contain viruses or bacteria that have been killed or inactivated so they can no longer cause disease. These vaccines require multiple doses to achieve and maintain immunity, as they may not induce as strong a response as live-attenuated vaccines. The polio vaccine is an example of an inactivated vaccine, and it has been crucial in reducing polio cases worldwide.
Then we have the innovative mRNA vaccines, which represent a significant advancement in vaccine technology. These vaccines use messenger RNA to instruct cells to produce a harmless piece of the virus's spike protein, triggering an immune response. The Pfizer-BioNTech and Moderna COVID-19 vaccines are notable examples. The beauty of mRNA vaccines lies in their ability to be developed rapidly and their potential for adaptability against emerging pathogens.
Other types of vaccines include subunit, recombinant, and toxoid vaccines. Subunit vaccines contain only parts of the virus or bacteria, such as proteins, which can stimulate an immune response without introducing the whole pathogen. Recombinant vaccines use genetic engineering to produce antigens in a lab, while toxoid vaccines contain inactivated toxins produced by bacteria, like the diphtheria and tetanus vaccines. Each of these types plays a vital role in our overall vaccination strategy, providing options tailored to different diseases and populations.
In conclusion, understanding the various types of vaccines is crucial for appreciating their significance in preventing diseases. Whether through live-attenuated, inactivated, or newer mRNA technologies, vaccines harness the body's immune response to provide protection against potentially severe infections. As we continue to innovate in vaccine development, it’s essential to stay informed about their types and functions to make educated decisions about our health and the health of our communities.
- What is the difference between live-attenuated and inactivated vaccines?
Live-attenuated vaccines use weakened forms of pathogens, while inactivated vaccines use killed pathogens. - How do mRNA vaccines work?
mRNA vaccines instruct cells to produce a harmless piece of the virus's spike protein, prompting an immune response. - Are there any side effects from vaccines?
Some people may experience mild side effects like soreness at the injection site, fatigue, or mild fever, but these are usually temporary. - Why do some vaccines require multiple doses?
Some vaccines need multiple doses to build and maintain adequate immunity over time.

When it comes to vaccines, the terms efficacy and safety are paramount. Understanding these concepts can empower you to make informed decisions about your health and the health of your loved ones. Vaccine efficacy refers to the ability of a vaccine to provide protection against a specific disease under controlled conditions, such as clinical trials. For example, if a vaccine shows 95% efficacy, it means that out of 100 people vaccinated, 95 will be protected from the disease. This high level of protection is crucial in controlling outbreaks and preventing the spread of infectious diseases.
However, efficacy alone does not paint the complete picture. Vaccine safety is equally important and is rigorously assessed before any vaccine is approved for public use. Regulatory agencies, like the FDA in the United States, conduct extensive testing to ensure that vaccines do not cause harmful side effects. These tests are conducted in multiple phases, where thousands of volunteers receive the vaccine and are monitored for any adverse reactions. Only after thorough examination and analysis can a vaccine be deemed safe for the general population.
It's also essential to understand that while vaccines are generally safe, some individuals may experience mild side effects, such as soreness at the injection site, low-grade fever, or fatigue. These reactions are typically short-lived and indicate that the immune system is responding to the vaccine. Serious side effects are extremely rare, and the benefits of vaccination far outweigh the risks for the vast majority of people.
Moreover, the ongoing monitoring of vaccine safety continues even after a vaccine is approved. Systems like the Vaccine Adverse Event Reporting System (VAERS) in the U.S. allow healthcare providers and the public to report any adverse effects following vaccination. This data helps health authorities track any potential safety concerns and take appropriate action if necessary.
In summary, vaccines undergo rigorous testing to ensure both their efficacy and safety. The ongoing evaluation of vaccine performance in real-world conditions further strengthens our confidence in their role in public health. Vaccination not only protects individuals but also contributes to herd immunity, helping to shield those who cannot be vaccinated due to medical reasons.
- What is vaccine efficacy? Vaccine efficacy is a measure of how well a vaccine works in preventing disease under ideal conditions.
- Are vaccines safe? Yes, vaccines go through extensive testing and monitoring to ensure they are safe for public use.
- What are common side effects of vaccines? Mild side effects may include soreness at the injection site, fever, or fatigue, but serious side effects are rare.
- How is vaccine safety monitored? Vaccine safety is continuously monitored through reporting systems like VAERS, where adverse effects can be reported and analyzed.
Frequently Asked Questions
- What is the immune system and why is it important?
The immune system is like your body's security team, constantly on the lookout for harmful invaders like bacteria and viruses. It plays a crucial role in protecting your body from diseases and maintaining overall health. Without a well-functioning immune system, even minor infections could become serious problems.
- What are the main types of immunity?
There are two primary types of immunity: innate and adaptive. Innate immunity is your body's first line of defense, responding quickly to any threat, while adaptive immunity takes a bit longer to kick in but provides a targeted response to specific pathogens, thanks to memory cells that remember past infections.
- How do physical barriers contribute to innate immunity?
Physical barriers, such as your skin and mucous membranes, act like a fortress wall, preventing pathogens from entering your body. They are essential for maintaining health by blocking the entry of harmful microorganisms and providing a first line of defense.
- What are autoimmune diseases?
Autoimmune diseases occur when the immune system mistakenly attacks healthy cells, thinking they are invaders. This can lead to various health issues, as the body essentially turns against itself. Managing these diseases often requires specialized treatment to help control the immune response.
- How does nutrition impact immune health?
Your diet is like fuel for your immune system. Eating a balanced diet rich in vitamins and minerals, such as vitamin C, D, and zinc, can enhance your immune function and help your body fight off infections more effectively.
- What role does exercise play in immune function?
Regular exercise is like a booster shot for your immune system! It improves circulation, enhances immune responses, and helps your body fend off infections. Staying active is a key factor in maintaining a robust immune system.
- Why is sleep important for immunity?
Sleep is your body's time to recharge and repair. Without enough sleep, your immune system may not function optimally, making you more susceptible to infections. Think of sleep as your immune system's secret weapon for staying strong and healthy!
- How do vaccines enhance immune function?
Vaccines train your immune system to recognize and combat specific pathogens. By introducing a harmless part of the virus or bacteria, vaccines stimulate your immune response, creating memory cells that help protect you from future infections.
- Are vaccines safe and effective?
Yes! Vaccines undergo rigorous testing to ensure their safety and efficacy before they are approved for public use. Understanding the science behind vaccines helps you make informed decisions about your health and contributes to community immunity.