The Biology of Eating Disorders - Understanding Causes
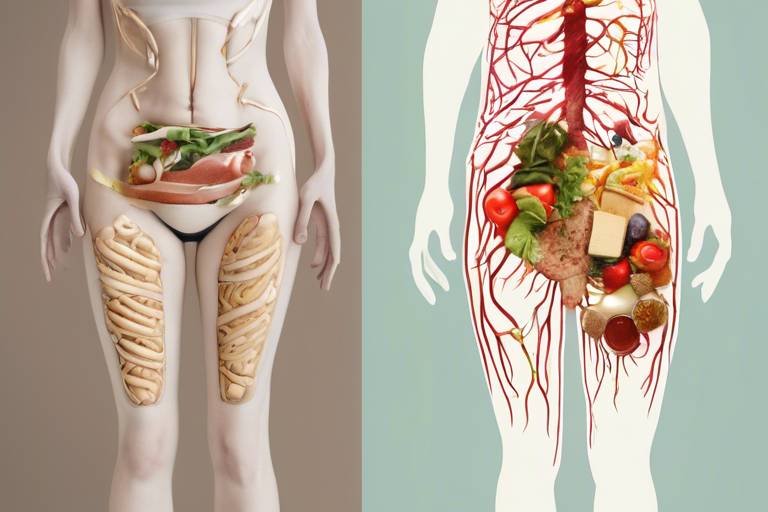
Eating disorders are complex conditions that intertwine biology, psychology, and environment. Understanding the biological underpinnings of these disorders is essential for grasping why certain individuals may develop them. This article dives deep into the genetic, neurobiological, and environmental factors that contribute to eating disorders, shedding light on how they affect individuals' health. By exploring these facets, we can better appreciate the intricate dance between our biology and the world around us, ultimately leading to more effective treatments and support systems.
Genetics play a pivotal role in the development of eating disorders. Research suggests that individuals may inherit certain genetic predispositions that heighten their vulnerability to these conditions. For instance, variations in specific genes can influence behaviors related to eating and body image perceptions. Imagine genetics as a blueprint; while it sets the foundation, environmental factors can shape the final structure. Studies indicate that if a family has a history of eating disorders, the likelihood of other members developing similar issues increases significantly.
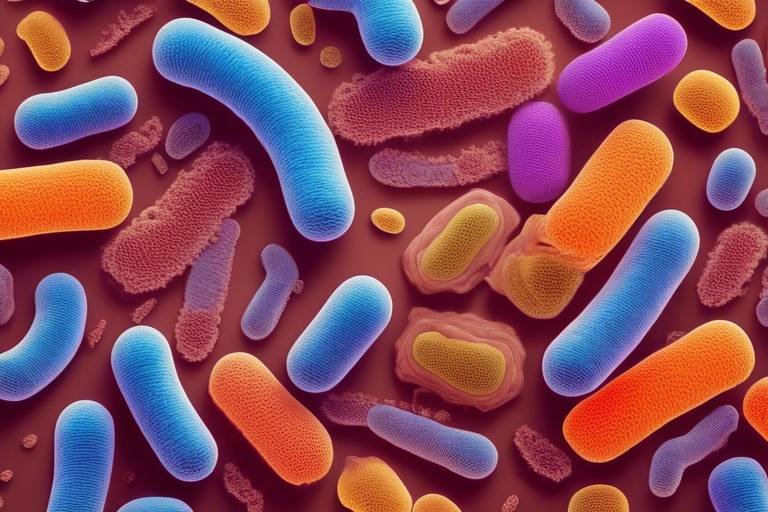
Neurotransmitters, the brain's chemical messengers, are crucial in regulating mood and appetite. Among these, serotonin and dopamine stand out as key players in the realm of eating disorders. An imbalance in these neurochemicals can lead to a cascade of emotional and behavioral issues, potentially triggering or exacerbating disordered eating patterns. Understanding how these chemicals function gives us insight into the emotional landscape of individuals suffering from eating disorders.
Serotonin is often referred to as the "feel-good" neurotransmitter, playing a vital role in mood regulation and appetite control. When serotonin levels are low, individuals may experience heightened anxiety and depression, which can trigger disordered eating behaviors. Think of serotonin as a stabilizing force; when it's lacking, the emotional equilibrium can be thrown off, leading to unhealthy coping mechanisms such as binge eating or restrictive diets.
Dopamine is another critical neurotransmitter involved in the brain's reward system. It helps us experience pleasure, including the enjoyment derived from eating. However, when dopamine pathways are dysregulated, individuals may find themselves caught in a cycle of binge eating or food restriction. This dysregulation can alter how one perceives food, transforming it from a source of nourishment into a battleground of emotional struggle.
Neurochemical imbalances can also disrupt the body's natural hunger signals. When these signals are distorted, individuals may struggle to recognize their body's needs. This confusion can lead to unhealthy eating patterns, where individuals either overeat or undereat, ignoring the body's cues. It's like trying to tune into a radio station with poor reception; the signals are there, but they’re jumbled and unclear, making it difficult to understand what the body truly requires.
Research has shown that certain structural and functional differences in the brain may predispose individuals to eating disorders. These differences can affect key aspects such as decision-making, impulse control, and emotional regulation. For example, individuals with altered brain structures may find it challenging to resist unhealthy food choices or cope with emotional distress, leading to a higher risk of developing disordered eating behaviors. It's like having a faulty compass; even with the right map, one may struggle to find the correct path.
While biological factors play a significant role, environmental influences cannot be overlooked. Societal pressures, cultural ideals, and traumatic experiences can interact with genetic predispositions, increasing the risk of developing eating disorders. These environmental triggers often amplify the vulnerabilities created by genetic and neurochemical factors, creating a perfect storm for disordered eating to flourish.
Cultural ideals surrounding body image and beauty significantly impact self-esteem and body dissatisfaction. In a society that often equates thinness with success and happiness, individuals may feel compelled to engage in disordered eating behaviors to meet these unrealistic standards. This societal pressure can act as a catalyst, pushing individuals toward unhealthy eating habits in an attempt to conform to an ideal that is often unattainable.
Life's stressful events, such as trauma, loss, or significant life changes, can serve as triggers for eating disorders, especially in those with a genetic vulnerability or pre-existing mental health issues. When faced with overwhelming stress, some individuals may turn to food as a source of comfort, while others may restrict their intake as a means of exerting control. It’s like a pressure cooker; without healthy outlets for stress, the internal pressures can lead to explosive outcomes in the form of disordered eating.
- What are the most common types of eating disorders? The most common types include anorexia nervosa, bulimia nervosa, and binge eating disorder.
- Can eating disorders be treated? Yes, with the right combination of therapy, medical treatment, and support, many individuals can recover from eating disorders.
- How can I help someone with an eating disorder? Encourage open communication, offer support, and suggest professional help without being judgmental.

Genetic Factors
When we delve into the intricate world of eating disorders, one cannot overlook the profound impact of . It's fascinating to consider that our very DNA could be a key player in shaping our relationship with food and body image. Research has shown that certain genes can predispose individuals to these complex conditions, making them more susceptible to disordered eating behaviors. Imagine your genetic makeup as a blueprint; it doesn't dictate every choice you make, but it certainly influences the structure and function of your body, including aspects related to eating.
For instance, studies have identified specific genetic markers that correlate with behaviors often seen in eating disorders, such as impulsivity and anxiety. These traits can create a perfect storm for developing conditions like anorexia nervosa or bulimia. It's like having a predisposition to a talent; while not everyone with the gene will become a concert pianist, the potential is there, waiting for the right circumstances to flourish.
Moreover, the interplay of genetics with environmental factors is crucial. Think of it as a dance between nature and nurture. An individual might have a genetic vulnerability, but without certain environmental triggers—like societal pressures or traumatic experiences—these predispositions may never manifest into a full-blown eating disorder. This complex relationship highlights the need for a comprehensive understanding of how our biology interacts with our surroundings.
To further illustrate this point, let's consider a table that summarizes some of the key genetic factors associated with eating disorders:
| Genetic Factor | Associated Eating Disorder | Impact |
|---|---|---|
| 5-HTTLPR | Bulimia Nervosa | Influences serotonin levels affecting mood and appetite. |
| BDNF | Anorexia Nervosa | Affects brain function related to eating behaviors. |
| COMT | General Eating Disorders | Impacts dopamine metabolism, influencing reward processing. |
As we can see, these genetic factors play a significant role in shaping the likelihood of developing eating disorders. However, it's essential to remember that genetics alone does not determine destiny. Just as a seed needs the right soil, water, and sunlight to grow, individuals with genetic predispositions require a supportive environment to thrive. In the absence of negative influences, those with genetic vulnerabilities may lead healthy, balanced lives.
In conclusion, while genetics significantly contribute to the risk of eating disorders, they are just one piece of a much larger puzzle. Understanding this complexity is vital for developing effective prevention and treatment strategies. By acknowledging the biological underpinnings of these conditions, we can better support individuals struggling with eating disorders in their journey toward recovery.

Neurochemical Influences
When we delve into the world of eating disorders, one of the most fascinating yet complex aspects is the role of . Our brains are intricate networks of neurotransmitters, which are like the body's chemical messengers, regulating everything from mood to appetite. Among these, two players stand out: serotonin and dopamine. These neurotransmitters are not just random chemicals floating around; they are pivotal in shaping our behaviors and emotional states, particularly when it comes to how we relate to food.
First, let’s talk about serotonin. This neurotransmitter is often referred to as the "feel-good" chemical because of its profound impact on mood regulation. Imagine serotonin as the conductor of an orchestra, harmonizing our emotions and appetite. When serotonin levels are low, it can lead to a cacophony of issues, including increased anxiety and depression. This emotional turmoil can trigger disordered eating behaviors as individuals may turn to food for comfort or, conversely, restrict their intake in an attempt to regain control. It's a vicious cycle that can be hard to break.
Low serotonin levels can create a perfect storm for disordered eating. Picture this: you’re feeling down, and suddenly, that piece of chocolate cake looks like the solution to all your problems. But the relief is temporary, and soon you find yourself spiraling into patterns of binge eating or restrictive dieting. This is where the connection between serotonin and eating disorders becomes crystal clear. The brain’s chemistry can profoundly influence our choices, leading us down paths that are difficult to navigate.
Now, let’s shift our focus to dopamine. Often dubbed the "pleasure chemical," dopamine is crucial for the brain's reward system. Think of it as the fuel that drives our desire for food, pleasure, and satisfaction. When we eat something delicious, dopamine is released, creating a sense of joy and reward. However, if there’s a dysregulation in these dopamine pathways, the experience can change drastically. For some individuals, this might manifest as binge eating, where the quest for pleasure from food becomes overwhelming. They might find themselves eating not because they are hungry, but because they are chasing that fleeting dopamine high.
In fact, the interplay between serotonin and dopamine can create a complicated web of cravings and emotional responses. If serotonin levels are low and dopamine pathways are dysregulated, individuals may struggle to find balance in their eating habits. This disruption can make it incredibly challenging to listen to the body’s natural hunger signals, leading to unhealthy eating patterns that further exacerbate the issue.
Speaking of hunger signals, neurochemical imbalances can wreak havoc on how we perceive our body's needs. Imagine trying to tune into a radio station, but the signal is fuzzy and intermittent. That’s what it’s like for someone with disrupted neurochemistry trying to recognize hunger cues. They might ignore their body's signals altogether, leading to extreme hunger or, conversely, a lack of appetite. This miscommunication can set the stage for a range of eating disorders, as individuals struggle to find a healthy relationship with food.
In summary, the neurochemical influences on eating disorders are profound and multifaceted. Understanding the roles of serotonin and dopamine not only sheds light on the biological underpinnings of these conditions but also highlights the importance of addressing mental health in treatment plans. By recognizing the intricate dance between our brain chemistry and eating behaviors, we can begin to unravel the complexities of eating disorders and pave the way for more effective interventions.
- What are eating disorders? Eating disorders are serious mental health conditions characterized by unhealthy eating habits and preoccupations with food, body weight, and shape.
- How do neurotransmitters affect eating behaviors? Neurotransmitters like serotonin and dopamine play crucial roles in regulating mood and appetite. Imbalances can lead to disordered eating patterns.
- Can eating disorders be treated? Yes, eating disorders can be treated through a combination of therapy, nutritional counseling, and medical support.
- What is the role of genetics in eating disorders? Genetic predispositions can increase vulnerability to eating disorders, interacting with environmental factors to influence their development.

Serotonin's Role
When we talk about serotonin, we’re diving into a world that intertwines our mood, appetite, and overall mental health. This neurotransmitter, often dubbed the "feel-good" chemical, plays a crucial role in regulating not just how we feel but also how we eat. Imagine serotonin as a conductor of an orchestra, harmonizing various elements of our brain to create a balanced melody. However, when the levels of serotonin drop, this symphony can quickly turn into a chaotic cacophony, leading to increased anxiety and depression.
Low serotonin levels can be a double-edged sword. On one hand, they can fuel feelings of sadness and hopelessness, which might push someone toward unhealthy eating behaviors as a form of coping. On the other hand, they can also trigger a vicious cycle: poor mood leads to disordered eating, which in turn can further deplete serotonin levels. It’s like a hamster wheel that just won’t stop, making it challenging for individuals to break free from these patterns.
Furthermore, serotonin is intricately linked to our appetite control. Research has shown that when serotonin levels are low, individuals may experience heightened cravings for carbohydrates, which can lead to binge eating episodes. This craving is not just a simple desire; it’s a biological response aimed at restoring serotonin levels, as carbohydrates can temporarily boost serotonin production. Thus, the relationship between serotonin and eating behaviors is complex and multifaceted.
To illustrate this point, consider the following table that summarizes the effects of serotonin on mood and appetite:
| Serotonin Level | Mood Impact | Appetite Response |
|---|---|---|
| High | Stable, positive | Balanced appetite |
| Normal | Generally content | Regular eating patterns |
| Low | Increased anxiety, depression | Heightened cravings, disordered eating |
In summary, serotonin is not just a player in the game of mood regulation; it’s a key factor in how we approach food and eating. Understanding its role can shed light on why individuals with eating disorders often struggle with their relationship with food. By recognizing the biological underpinnings of these conditions, we can begin to address the emotional and mental health aspects that contribute to disordered eating.
- What is serotonin? Serotonin is a neurotransmitter that helps regulate mood, appetite, and sleep.
- How does serotonin affect eating disorders? Low serotonin levels can lead to increased anxiety and cravings for carbohydrates, contributing to disordered eating behaviors.
- Can serotonin levels be increased naturally? Yes, regular exercise, a balanced diet, and exposure to sunlight can help boost serotonin levels.

Dopamine and Reward Pathways
Dopamine is often referred to as the "feel-good" neurotransmitter, and for good reason! It plays a pivotal role in the brain's reward system, which is essentially a complex network that influences our feelings of pleasure and motivation. When we engage in activities that are pleasurable—like eating delicious food—dopamine is released, reinforcing that behavior and encouraging us to repeat it. However, this intricate balance can be disrupted, particularly in individuals with eating disorders.
In the context of eating disorders, the dysregulation of dopamine pathways can lead to significant challenges. For instance, if dopamine levels are too low, individuals may not experience the same sense of satisfaction from food, which could lead them to eat more in an attempt to achieve that pleasurable feeling. Conversely, if the dopamine system is overly sensitive, it might cause an individual to derive excessive pleasure from food, potentially resulting in binge eating episodes. This rollercoaster of reward and pleasure can create a vicious cycle that is hard to break.
Moreover, the way dopamine interacts with other neurotransmitters can further complicate the scenario. For example, an imbalance in serotonin levels can also affect dopamine function, leading to even more profound implications for mood and appetite regulation. This interplay between neurotransmitters is crucial because it highlights how the brain's chemistry can influence eating behaviors. Understanding these pathways can provide insight into why some individuals may turn to food as a coping mechanism in response to stress or emotional turmoil.
To illustrate the impact of dopamine dysregulation further, consider the following table that outlines the potential effects of dopamine imbalance on eating behaviors:
| Dopamine Level | Possible Effect on Eating Behavior |
|---|---|
| Low | Decreased pleasure from food; potential for binge eating to seek satisfaction |
| High | Increased pleasure from food; risk of binge eating or compulsive eating behaviors |
In summary, the relationship between dopamine and the brain's reward pathways is a critical factor in understanding eating disorders. By recognizing how dopamine influences our eating habits, we can better comprehend the challenges faced by individuals struggling with these conditions. This knowledge may pave the way for more effective treatments that address the underlying neurochemical imbalances, ultimately helping individuals regain control over their eating behaviors.
- What is the role of dopamine in eating disorders? Dopamine influences the brain's reward system, affecting how pleasure is derived from food and can lead to unhealthy eating behaviors when imbalanced.
- How does dopamine dysregulation affect hunger signals? An imbalance in dopamine can disrupt normal hunger signals, making it difficult for individuals to recognize their body's needs.
- Can dopamine levels be adjusted? Yes, lifestyle changes, therapy, and medication can help regulate dopamine levels and improve overall mental health.

Impact on Hunger Signals
When we think about eating, we often focus on what we eat and how much. However, the is a crucial aspect that often goes unnoticed, especially in the context of eating disorders. Neurochemical imbalances can significantly disrupt the body's natural hunger cues, leaving individuals feeling confused about their own needs. Imagine your body as a finely tuned orchestra, where each instrument plays its part to create a harmonious melody. Now, picture that orchestra suddenly going out of tune—this is what happens when hunger signals are disrupted.
For instance, individuals with eating disorders may struggle to identify when they are truly hungry or full. This miscommunication can lead to a vicious cycle of overeating or undereating. When the brain's neurochemical pathways are altered, it can create a disconnect between the physical sensations of hunger and the emotional responses to those sensations. This disconnection can be likened to a car with a faulty GPS; you might know you need to eat, but you have no idea how to get there.
Moreover, the inability to recognize hunger signals can lead to a range of unhealthy eating patterns. Some individuals might resort to binge eating, where they consume large amounts of food in a short period, often in response to emotional triggers rather than genuine hunger. Others might experience restriction, ignoring their body's signals entirely, believing that they should not eat at all. This tug-of-war between the mind and body can create a chaotic relationship with food, making it even more challenging to establish a healthy eating pattern.
To further illustrate this, consider the following table that summarizes how neurochemical imbalances can affect hunger signals:
| Neurotransmitter | Impact on Hunger Signals |
|---|---|
| Serotonin | Low levels can lead to increased anxiety and depression, affecting appetite control. |
| Dopamine | Dysregulation can alter the experience of pleasure from food, impacting eating behavior. |
| Ghrelin | Imbalances may disrupt the signal that indicates hunger, leading to overeating or undereating. |
| Leptin | Resistance to leptin can impair the ability to recognize fullness, causing excessive eating. |
In conclusion, the is a complex interplay between neurochemistry and behavior. Understanding this relationship is essential for those struggling with eating disorders, as it can pave the way for more effective treatment approaches. By addressing these neurochemical imbalances, individuals can begin to reconnect with their body's natural signals, fostering a healthier relationship with food.
- What are the main causes of eating disorders? Eating disorders can be caused by a combination of genetic, neurobiological, and environmental factors.
- How can neurochemical imbalances affect eating behavior? Imbalances in neurotransmitters like serotonin and dopamine can disrupt hunger signals and emotional regulation, leading to disordered eating.
- Can eating disorders be treated effectively? Yes, with a combination of therapy, nutritional counseling, and medical support, many individuals can recover from eating disorders.

Brain Structure and Function
The human brain is a complex organ, and its structure and function play a pivotal role in the development of eating disorders. Research has shown that certain anatomical differences in the brain can predispose individuals to these conditions. For instance, variations in areas such as the prefrontal cortex and the amygdala can significantly affect how one processes emotions, makes decisions, and regulates impulses. The prefrontal cortex is crucial for executive functions like planning and self-control, while the amygdala is involved in emotional responses. When these areas function atypically, individuals may struggle to manage their emotions, leading to unhealthy coping mechanisms like disordered eating.
Moreover, brain imaging studies have indicated that individuals with eating disorders often exhibit altered brain activity in regions associated with reward processing and self-regulation. Functional MRI scans reveal that those with conditions such as anorexia nervosa or bulimia nervosa may have heightened activity in the brain's reward pathways when they engage in restrictive eating or bingeing behaviors. This can create a vicious cycle where the brain's response to food becomes increasingly distorted, reinforcing unhealthy eating patterns.
To further understand the relationship between brain structure and eating disorders, it’s essential to consider the following key aspects:
- Decision-Making: Impaired decision-making abilities can lead to poor choices regarding food intake and body image.
- Impulse Control: An inability to control impulses can result in binge eating or purging behaviors.
- Emotional Regulation: Difficulty in managing emotions can trigger disordered eating as a means of coping.
Additionally, the connectivity between different brain regions can influence how individuals experience hunger and satiety. For example, disruptions in the communication between the hypothalamus, which regulates hunger signals, and the prefrontal cortex can lead to a disconnect between what the body needs and what the individual perceives. This miscommunication can manifest as extreme hunger or a complete disregard for hunger cues, paving the way for eating disorders.
In summary, understanding the biological underpinnings of eating disorders, particularly through the lens of brain structure and function, highlights the complexity of these conditions. It’s not merely about food or weight; it’s a multifaceted interplay of genetics, neurochemistry, and brain architecture that shapes how individuals relate to their bodies and food.
- What are the main causes of eating disorders? Eating disorders stem from a combination of genetic, neurobiological, and environmental factors, including societal pressures and personal experiences.
- How do neurotransmitters affect eating behaviors? Neurotransmitters like serotonin and dopamine influence mood and appetite, and imbalances can lead to disordered eating patterns.
- Can brain structure influence eating disorders? Yes, structural differences in the brain can affect decision-making, impulse control, and emotional regulation, contributing to the risk of developing eating disorders.
- What role does environment play in eating disorders? Environmental factors, such as cultural ideals and psychological stressors, can interact with biological predispositions to trigger eating disorders.

Environmental Triggers
When we dive into the world of eating disorders, it's essential to understand that biology isn't the only player in this complex game. can significantly influence the onset and progression of these disorders. Imagine a seed planted in fertile soil; while the seed's genetic makeup is crucial, the environment in which it grows can determine whether it flourishes or withers away. This analogy perfectly encapsulates the interplay between genetic predispositions and environmental factors.
One of the most potent environmental influences comes from societal pressures. In today's world, we are bombarded with images and messages that glorify unrealistic body standards. Think about it: social media platforms often showcase edited and filtered images that present a narrow definition of beauty. This can lead to a toxic cycle where individuals constantly compare themselves to these idealized versions, resulting in body dissatisfaction. When people feel that they don't measure up, it can trigger disordered eating behaviors as a misguided attempt to achieve that 'perfect' body. The impact of these societal ideals is profound, affecting not just self-esteem but also mental health.
Furthermore, psychological stressors play a crucial role in the development of eating disorders. Life is full of challenges, and for some, these challenges can be overwhelming. Events such as trauma, loss, or significant life changes can act as catalysts for disordered eating, particularly in those who may already carry a genetic vulnerability. For instance, someone who has experienced trauma might turn to food as a coping mechanism, leading to binge eating. Alternatively, they might restrict their food intake as a way to exert control over their lives when everything else feels chaotic. This duality highlights how environmental stressors can intertwine with biological factors to create a perfect storm for eating disorders.
Additionally, peer influence cannot be overlooked. Friends and social circles can either be a source of support or a breeding ground for unhealthy behaviors. If someone is surrounded by peers who prioritize thinness or engage in dieting culture, they may feel pressured to conform. This can lead to a cycle of negative body image and unhealthy eating behaviors, reinforcing the idea that one must look a certain way to be accepted.
In summary, while genetics and neurobiology lay the groundwork, it is the environmental triggers that often pull the strings. Understanding this intricate web of influences is crucial for addressing eating disorders effectively. By recognizing the societal pressures, psychological stressors, and peer influences that can trigger these conditions, we can begin to foster a more supportive environment for those struggling. Acknowledging these factors is the first step toward prevention and recovery.
- What are some common environmental triggers for eating disorders? Environmental triggers can include societal pressures, cultural ideals of beauty, psychological stressors, and peer influence.
- How can societal pressures affect body image? Societal pressures can create unrealistic standards of beauty, leading to body dissatisfaction and potentially triggering disordered eating behaviors.
- Can trauma lead to eating disorders? Yes, traumatic experiences can act as significant triggers for eating disorders, particularly in individuals with a genetic predisposition.
- How can I support someone with an eating disorder? Providing a supportive and non-judgmental environment, encouraging open conversations, and promoting a healthy relationship with food can be beneficial.

Societal Influences
When we think about eating disorders, it’s easy to focus solely on the individual’s biology or psychology. However, we mustn't overlook the powerful impact of . From a young age, we are bombarded with messages about what our bodies should look like, how much we should weigh, and what it means to be "healthy." These cultural ideals can warp our perceptions and expectations, leading many to engage in disordered eating as they chase after these often unrealistic standards.
Consider this: the media plays a crucial role in shaping our ideas of beauty. With the rise of social media, we are constantly exposed to images of seemingly perfect bodies, filtered to perfection. This exposure can create a distorted view of reality, making individuals feel inadequate or dissatisfied with their own bodies. As a result, many may resort to unhealthy eating habits in an attempt to achieve the unattainable.
Moreover, societal norms surrounding thinness and beauty can create an environment where individuals feel pressured to conform. For instance, in many cultures, being thin is equated with success, happiness, and even morality. This pressure can be overwhelming, especially for young people who are still forming their identities. The desire to fit in or be accepted can lead to dangerous behaviors, such as extreme dieting or excessive exercising.
Additionally, the influence of peers cannot be underestimated. Friends and family can either support healthy behaviors or perpetuate harmful ones. In a society that often prioritizes appearance over health, conversations about weight and body image can become toxic. For example, a simple comment about someone’s weight can trigger a cascade of negative thoughts and behaviors. It’s essential to foster an environment where individuals feel safe and accepted, regardless of their size.
To illustrate the impact of societal influences, here’s a table that outlines some key factors:
| Factor | Impact |
|---|---|
| Media Representation | Promotes unrealistic body standards and ideals. |
| Cultural Norms | Associates thinness with success and moral character. |
| Peer Pressure | Encourages unhealthy comparisons and behaviors. |
| Social Media | Increases exposure to edited images, leading to body dissatisfaction. |
In conclusion, societal influences are a significant factor in the development of eating disorders. They weave a complex web of expectations that can trap individuals into harmful cycles of behavior. By recognizing and addressing these societal pressures, we can begin to dismantle the harmful narratives surrounding body image and promote a culture that values health over appearance.
- What are the main societal factors contributing to eating disorders?
Media representation, cultural norms, peer pressure, and social media are significant factors that contribute to the development of eating disorders.
- How can we combat societal pressures related to body image?
Promoting body positivity, fostering open conversations about health, and encouraging diverse representations in media can help combat these pressures.
- What role do friends and family play in eating disorders?
Friends and family can either support healthy behaviors or perpetuate harmful ones through comments and expectations about body image.

Psychological Stressors
Psychological stressors are like the hidden monsters lurking in the shadows of our minds, often triggering a cascade of emotional turmoil that can lead to eating disorders. Imagine a pressure cooker: when it builds up too much heat without a way to release it, it can explode. Similarly, when individuals face overwhelming stress from life events, their coping mechanisms can falter, leading to disordered eating behaviors as a means of escape or control.
Stressful life events can take many forms, including trauma, loss, or significant changes in one's life circumstances. For example, the loss of a loved one can create a sense of emptiness or despair, prompting individuals to seek solace in food, whether through binge eating or restrictive diets. It's as if food becomes a comforting blanket, providing temporary relief from emotional pain. However, this relief is often fleeting and can spiral into a cycle of guilt and shame, further exacerbating the disorder.
Moreover, individuals with a genetic predisposition to mental health issues may find themselves more susceptible to these stressors. A person who has experienced trauma may not only deal with the emotional fallout but also grapple with a biological vulnerability that makes them more likely to turn to food as a coping mechanism. This interplay between and biological factors creates a complex web that can be challenging to untangle.
To illustrate the impact of psychological stressors on eating disorders, consider the following table that outlines common stressors and their potential effects:
| Common Psychological Stressors | Potential Effects on Eating Behaviors |
|---|---|
| Trauma (e.g., abuse, accidents) | Increased likelihood of binge eating or restrictive behaviors as coping mechanisms |
| Loss of a loved one | Emotional eating to fill the void or avoid grief |
| Major life changes (e.g., divorce, moving) | Disordered eating as a way to regain control in an unstable environment |
| Chronic stress (e.g., work-related) | Using food as a comfort during high-pressure situations |
It's crucial to recognize that while these stressors can trigger disordered eating, they do not operate in isolation. The social environment, cultural expectations, and individual personality traits also play significant roles. For instance, someone who feels immense pressure to conform to societal beauty standards may react to stress by engaging in extreme dieting or binge eating, further complicating their relationship with food.
In conclusion, psychological stressors are powerful catalysts for the development and maintenance of eating disorders. Understanding this connection is essential for effective treatment and support. By addressing both the psychological and biological aspects of these disorders, we can help individuals find healthier coping strategies and ultimately foster a more positive relationship with food and their bodies.
- What are common psychological stressors that lead to eating disorders?
Common stressors include trauma, loss of a loved one, major life changes, and chronic stress. - How do psychological stressors interact with genetic factors?
Individuals with a genetic predisposition to mental health issues may be more susceptible to the effects of psychological stressors, leading to disordered eating behaviors. - Can addressing psychological stressors help in treating eating disorders?
Yes, recognizing and addressing psychological stressors is crucial for effective treatment and support in overcoming eating disorders.
Frequently Asked Questions
- What are the main causes of eating disorders?
Eating disorders are complex conditions influenced by a mix of genetic, neurobiological, and environmental factors. Genetics can predispose individuals to these disorders, while neurotransmitters like serotonin and dopamine play significant roles in mood and appetite regulation. Environmental triggers, such as societal pressures and psychological stressors, can also exacerbate these conditions.
- How do genetic factors contribute to eating disorders?
Genetic predispositions can significantly affect behaviors and body image perceptions. Research shows that certain genes may increase vulnerability to developing eating disorders, making some individuals more susceptible than others. This genetic link highlights the importance of understanding family histories when addressing these conditions.
- What role do neurotransmitters play in eating disorders?
Neurotransmitters like serotonin and dopamine are crucial in regulating mood and appetite. An imbalance in these chemicals can lead to increased anxiety and depression, which may trigger disordered eating behaviors. For instance, low serotonin levels can disrupt emotional well-being, while dopamine dysregulation can affect how we experience pleasure from food.
- Can environmental factors trigger eating disorders?
Absolutely! Environmental factors, including societal ideals and psychological stressors, can interact with biological predispositions. Cultural pressures regarding body image can lead to dissatisfaction and unhealthy eating patterns, while traumatic events can act as catalysts for those already vulnerable to these disorders.
- How do societal influences affect eating disorders?
Societal influences, such as unrealistic beauty standards, can significantly impact self-esteem and body image. When individuals strive to meet these often unattainable ideals, it can lead to disordered eating as a way to cope with feelings of inadequacy or body dissatisfaction.
- What are the psychological stressors linked to eating disorders?
Psychological stressors, like trauma, loss, or significant life changes, can trigger eating disorders, especially in those who already have a genetic vulnerability or pre-existing mental health issues. These stressors can create a cycle of negative emotions and unhealthy coping mechanisms, further entrenching the disorder.