The Future of Telemedicine and Scientific Research
In recent years, the landscape of healthcare has undergone a seismic shift, largely driven by the rise of telemedicine. This innovative approach to healthcare delivery has not only transformed how patients interact with their providers but has also paved the way for groundbreaking advancements in scientific research. Imagine being able to consult your doctor from the comfort of your home, or researchers collaborating across continents without the need for travel. The future of telemedicine is not just about convenience; it's about enhancing the quality of care and making healthcare accessible to everyone, regardless of their location.
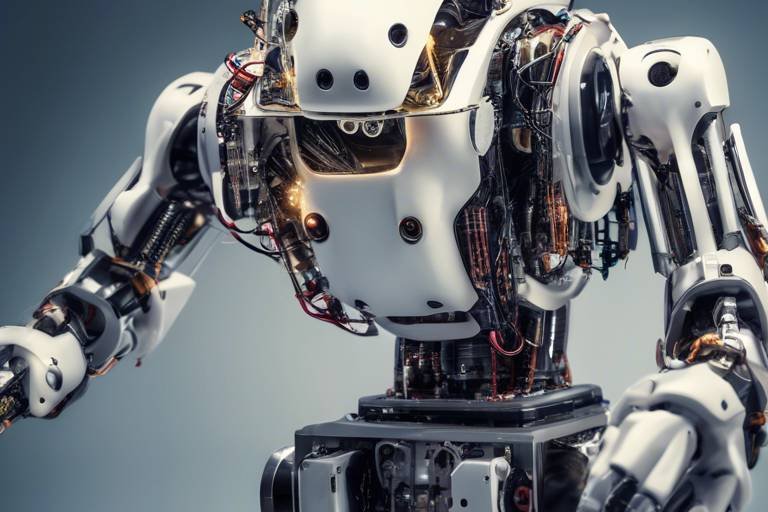
As we delve into the future of telemedicine, it's essential to understand the emerging technologies that are shaping this field. With the integration of artificial intelligence, wearable devices, and sophisticated telehealth platforms, the way we approach patient care is changing dramatically. These technologies not only enhance patient engagement but also streamline processes, allowing healthcare providers to monitor patients remotely and intervene when necessary. For instance, a patient with chronic conditions can be monitored via wearable technology that tracks vital signs, sending alerts to their healthcare team if any abnormalities arise. This proactive approach can lead to better health outcomes, reducing the need for emergency interventions.
Moreover, data plays a pivotal role in the telemedicine ecosystem. The collection and analysis of patient data enable healthcare providers to make informed decisions, ultimately leading to improved patient management and research capabilities. By harnessing the power of data analytics, telemedicine can offer personalized treatment plans tailored to individual needs. This not only enhances patient satisfaction but also fosters a more effective healthcare system. However, as we embrace these advancements, we must also address the challenges that come with them, including regulatory hurdles and technological barriers that may hinder the widespread adoption of telemedicine.
As telemedicine continues to evolve, it significantly impacts the dynamics of patient-provider relationships. Virtual consultations can alter traditional communication methods, raising questions about trust and satisfaction. How do we maintain strong relationships in a digital environment? Strategies such as ensuring clear communication, providing comprehensive follow-up care, and utilizing user-friendly technology can help bridge the gap between patients and providers, fostering a sense of connection even when face-to-face interactions are limited.
One of the most promising aspects of telemedicine is its potential to improve healthcare access for rural and underserved populations. For individuals living in remote areas, telemedicine can eliminate the barriers of distance and travel, making it easier to receive essential care. This is particularly important for those who may not have easy access to specialists or healthcare facilities. By addressing health disparities and providing equitable access to care, telemedicine can play a crucial role in enhancing the overall health of communities.
However, as we embrace the future of telemedicine, we must also confront ethical considerations surrounding privacy, consent, and equity. With the increasing reliance on technology comes the responsibility to ensure that telehealth practices are not only effective but also fair and just. Addressing these ethical dilemmas is vital for maintaining public trust and ensuring that the benefits of telemedicine are accessible to all.
Looking ahead, the future of telemedicine is brighter than ever. Emerging trends such as the integration of AI, personalized medicine, and advancements in remote patient monitoring technologies are set to reshape the healthcare landscape. The synergy between telemedicine and scientific research is particularly exciting, as telehealth facilitates data collection, patient recruitment, and collaboration among researchers across various fields. This interconnectedness can lead to faster advancements in medical knowledge and treatment options, ultimately benefiting patients worldwide.
In conclusion, the future of telemedicine and scientific research is not just about technology; it's about transforming lives. As we navigate this rapidly evolving field, we must embrace the opportunities it presents while remaining vigilant about the challenges that lie ahead. Together, we can create a healthcare system that is more accessible, efficient, and equitable for everyone.
- What is telemedicine? Telemedicine is the use of technology to provide healthcare services remotely, allowing patients to consult with healthcare providers via video calls, phone calls, or messaging.
- How does telemedicine benefit patients? Telemedicine offers convenience, improved access to specialists, and the ability to receive care without the need for travel, especially for those in rural or underserved areas.
- What technologies are commonly used in telemedicine? Common technologies include telehealth platforms, wearable devices, and mobile health applications that facilitate remote monitoring and communication.
- Are there any challenges associated with telemedicine? Yes, challenges include regulatory hurdles, technological barriers, and ethical considerations regarding privacy and equity in healthcare access.
- How does telemedicine impact scientific research? Telemedicine enhances scientific research by facilitating data collection, patient recruitment, and collaboration among researchers, leading to faster advancements in medical knowledge.

Emerging Technologies in Telemedicine
In the rapidly evolving world of healthcare, emerging technologies are reshaping the landscape of telemedicine, making it more efficient and accessible than ever before. Imagine being able to consult with a healthcare provider from the comfort of your home, while sophisticated algorithms analyze your health data in real time. This is no longer just a dream; it’s becoming a reality thanks to innovative technologies like artificial intelligence (AI), wearable devices, and advanced telehealth platforms.
AI is at the forefront of this revolution, utilizing machine learning to enhance diagnostic accuracy and personalize treatment plans. For instance, AI-powered chatbots can provide 24/7 patient support, answering queries and guiding individuals through their healthcare journeys. This technology not only saves time for both patients and providers but also ensures that no one feels alone in their health concerns. Furthermore, AI can analyze vast amounts of data to identify patterns, helping healthcare professionals make informed decisions that lead to better patient outcomes.
Wearable devices, such as fitness trackers and smartwatches, are another game-changer in telemedicine. These gadgets collect valuable health data, including heart rate, sleep patterns, and physical activity levels. Patients can share this information with their doctors in real time, allowing for continuous monitoring and timely interventions. For example, a patient with a chronic condition can be monitored remotely, reducing the need for frequent office visits while ensuring they receive the care they need. This kind of proactive approach not only enhances patient engagement but also leads to improved health management.
Telehealth platforms are evolving to offer comprehensive services that encompass everything from virtual consultations to remote patient monitoring. These platforms integrate multiple technologies, providing a seamless experience for both patients and healthcare providers. With features like secure messaging, video calls, and electronic health records, telehealth platforms facilitate effective communication and collaboration. Patients can easily schedule appointments, access their medical history, and communicate with their healthcare team, all from a single interface.
Moreover, the integration of Internet of Things (IoT) devices is expanding the capabilities of telemedicine. IoT devices can transmit health data directly to healthcare providers, allowing for real-time monitoring of patients with conditions such as diabetes or hypertension. This technology not only enhances patient care but also increases efficiency in healthcare delivery. By utilizing IoT, healthcare providers can respond quickly to any alarming changes in a patient's condition, potentially preventing serious complications.
As we look to the future, it is clear that the combination of these technologies will continue to transform telemedicine. The challenge lies in ensuring that these innovations are accessible to everyone, regardless of their location or socioeconomic status. By addressing these challenges head-on, we can pave the way for a more equitable healthcare system that leverages technology to improve health outcomes for all.

The Role of Data in Telemedicine
Data is the lifeblood of telemedicine, acting as a powerful engine that drives informed decision-making and enhances patient care. With the rapid advancement of technology, healthcare providers are now able to collect, analyze, and utilize vast amounts of data more efficiently than ever before. Imagine being able to pinpoint a patient's health trends over time, or predict potential health issues before they arise—this is the magic that data analytics brings to the table.
At the heart of telemedicine is the ability to gather data from various sources, including electronic health records (EHRs), wearable devices, and telehealth platforms. This data can be categorized into several types:
- Clinical Data: Information related to patient diagnosis, treatment plans, and outcomes.
- Behavioral Data: Insights into patient habits, adherence to treatment, and lifestyle choices.
- Operational Data: Metrics on service delivery, appointment scheduling, and resource utilization.
By leveraging these data types, healthcare providers can enhance patient management in several ways. For instance, predictive analytics can help identify patients at risk of chronic conditions, allowing for timely interventions. Additionally, data can facilitate personalized treatment plans that cater to individual patient needs, ultimately leading to better health outcomes.
Moreover, the integration of artificial intelligence (AI) into telemedicine platforms has opened new doors for data utilization. AI algorithms can sift through mountains of data to find patterns and correlations that human analysts might miss. This capability not only streamlines processes but also enriches the research landscape, enabling scientists to draw insights from real-world data.
However, the effective use of data in telemedicine isn't without its challenges. Issues such as data privacy, security, and interoperability of systems can hinder the seamless flow of information. Providers must navigate these challenges carefully, ensuring that patient data is protected while still being accessible for analysis. The importance of adhering to regulations like HIPAA in the United States cannot be understated, as these laws are designed to safeguard sensitive health information.
In summary, the role of data in telemedicine is multifaceted and crucial. It empowers healthcare providers to make informed decisions, enhances patient care, and drives scientific research forward. As we continue to embrace telemedicine, the potential for data analytics to transform healthcare is not just a possibility; it's an exciting reality that is unfolding before our eyes.
1. How does data analytics improve patient care in telemedicine?
Data analytics improves patient care by identifying trends, predicting health issues, and enabling personalized treatment plans, which leads to better health outcomes.
2. What types of data are collected in telemedicine?
Telemedicine collects clinical, behavioral, and operational data to enhance patient management and streamline healthcare processes.
3. What are the challenges associated with data use in telemedicine?
Challenges include data privacy and security concerns, as well as the need for interoperability among different healthcare systems.

Challenges Facing Telemedicine Adoption
As the world embraces the digital age, telemedicine stands out as a beacon of hope and innovation in healthcare. However, the road to widespread adoption is not without its bumps. One of the primary challenges is the regulatory landscape. Each country has its own set of laws and guidelines governing telehealth practices, which can create confusion for healthcare providers. For instance, some regions may require in-person consultations before telehealth services can be utilized, while others may have strict licensing requirements for practitioners. Navigating these regulations can be daunting, especially for smaller practices that may lack the resources to stay compliant.
Another significant hurdle is the technological barrier. Not all patients have access to the necessary technology or reliable internet connections. This digital divide can exacerbate existing health disparities, particularly in rural or underserved areas. Imagine trying to connect with a healthcare provider for a vital consultation, only to find that your internet connection is spotty or your device is outdated. Such scenarios can lead to frustration and missed opportunities for care.
Moreover, there's the issue of data security and privacy. With the rise of telemedicine, the amount of sensitive patient data being shared online has increased exponentially. This raises concerns about how securely this information is stored and transmitted. Patients may worry about their personal health information being compromised, leading to reluctance in utilizing telehealth services. It's essential for providers to implement robust security measures and educate patients on how their data is protected.
Additionally, the digital literacy of both patients and providers can impact the effectiveness of telemedicine. While many younger individuals are adept at using technology, older adults may struggle with navigating telehealth platforms. This can lead to a lack of engagement in their own care. Providers must be willing to offer support and guidance to ensure that all patients can effectively use these tools. For example, offering tutorials or having a dedicated support line can make a significant difference in patient comfort and confidence.
Lastly, the financial aspect cannot be overlooked. While telemedicine can reduce costs in the long run, the initial investment in technology and training can be substantial. Many healthcare systems are still grappling with reimbursement models that don't fully support telehealth services. Until there is a standardized approach to reimbursement, many providers may hesitate to fully embrace telemedicine.
In summary, while telemedicine offers a promising future for healthcare delivery, addressing these challenges is crucial for its successful implementation. By navigating regulatory complexities, bridging the technological divide, ensuring data security, enhancing digital literacy, and reevaluating financial models, we can pave the way for a more inclusive and effective telehealth landscape.
- What are the main challenges facing telemedicine adoption? The primary challenges include regulatory issues, technological barriers, data privacy concerns, digital literacy, and financial constraints.
- How can healthcare providers overcome these challenges? Providers can navigate regulations, invest in technology, enhance data security, offer support for digital literacy, and advocate for better reimbursement models.
- Why is digital literacy important in telemedicine? Digital literacy ensures that both patients and providers can effectively use telehealth platforms, leading to better engagement and health outcomes.

Impact on Patient-Provider Relationships
In the ever-evolving landscape of healthcare, the emergence of telemedicine has fundamentally altered the dynamics of patient-provider relationships. Traditionally, these relationships were built on face-to-face interactions, where the nuances of body language and personal connection played a significant role. However, with the rise of virtual consultations, we are witnessing a shift that brings both challenges and opportunities. So, how does telemedicine reshape the way patients and providers interact? Let's dive into the intricacies of this transformation.
One of the most significant impacts of telemedicine is the enhanced accessibility it provides. Patients can now consult with healthcare professionals from the comfort of their homes, breaking down geographical barriers that previously hindered access to quality care. For instance, individuals living in remote areas can connect with specialists who may not be available locally, thus fostering a sense of empowerment and engagement in their own health management. This newfound accessibility can lead to improved health outcomes, as patients are more likely to seek help when they can do so easily.
However, while accessibility is a major advantage, it also introduces new challenges regarding communication. In a virtual setting, the subtleties of in-person dialogue can sometimes be lost. Patients may struggle to convey their symptoms or concerns effectively through a screen, which can lead to misunderstandings or misdiagnoses. To mitigate these risks, providers must adapt their communication strategies. This includes asking open-ended questions and actively listening to ensure that patients feel heard and understood. The goal here is to maintain a strong rapport, even when the interaction lacks physical presence.
Moreover, the trust factor in patient-provider relationships is crucial. Trust is often built through consistent, personal interactions, and the transition to virtual care can pose a threat to this foundation. Patients may feel skeptical about the quality of care they are receiving or question the provider's ability to diagnose accurately without a physical examination. To foster trust in a telemedicine environment, healthcare providers must prioritize transparency and empathy. For example, they can take the time to explain the limitations of virtual consultations and reassure patients about the measures in place to ensure their safety and well-being.
Another interesting aspect of telemedicine is its potential to enhance patient engagement. With the availability of digital health tools, patients can take a more active role in their healthcare journey. They can monitor their health metrics using wearable devices and share this data with their providers in real-time. This collaborative approach not only empowers patients but also allows providers to tailor their recommendations based on comprehensive, up-to-date information. Ultimately, this partnership can lead to better adherence to treatment plans and improved health outcomes.
To sum it up, the impact of telemedicine on patient-provider relationships is multifaceted. While it presents challenges in terms of communication and trust, it also opens doors to greater accessibility and engagement. As we navigate this new terrain, both patients and providers must adapt to ensure that the essence of their relationship remains strong. By embracing the opportunities that telemedicine offers and addressing its challenges head-on, we can pave the way for a more connected and effective healthcare system.
- How does telemedicine affect the quality of care? Telemedicine can enhance the quality of care by providing timely access to healthcare professionals and enabling real-time monitoring of patients' health.
- Can telemedicine replace in-person visits? While telemedicine is a powerful tool, it may not replace in-person visits entirely. Certain conditions may still require physical examinations.
- What measures are in place to protect patient privacy in telemedicine? Telemedicine platforms typically use secure, encrypted connections to protect patient data and ensure confidentiality during consultations.

Telemedicine in Rural and Underserved Areas
Telemedicine is a game-changer for healthcare delivery, especially in rural and underserved areas. Imagine living in a small town, miles away from the nearest hospital, where every visit to a healthcare provider feels like an expedition. That’s the reality for many people. Telemedicine bridges this gap, allowing patients to connect with healthcare professionals from the comfort of their homes. This is not just a convenience; it's a lifeline for those who might otherwise go without essential medical care.
One of the most significant advantages of telemedicine in these regions is its ability to improve access to healthcare services. Patients can now schedule virtual appointments with specialists who may not be available locally. For instance, a farmer in a remote area can consult with a cardiologist in a bustling city without the need to travel hours. This not only saves time and money but also reduces the stress associated with long commutes, especially for those with mobility issues.
Moreover, telemedicine helps to reduce health disparities. Many rural communities face challenges such as limited healthcare facilities, a shortage of healthcare professionals, and higher rates of chronic diseases. By leveraging technology, telemedicine can deliver vital health services to these populations, ensuring that they receive timely diagnoses and treatments. For example, chronic conditions like diabetes and hypertension can be managed more effectively through regular virtual check-ins, allowing healthcare providers to monitor patients’ conditions closely and make necessary adjustments to their treatment plans.
However, it’s essential to recognize that the implementation of telemedicine in these areas is not without its challenges. Issues such as internet connectivity and technological literacy can hinder the effectiveness of telehealth services. In many rural regions, high-speed internet access is still a luxury, making it difficult for patients to participate in video consultations. Furthermore, not everyone is comfortable using technology, which can create barriers to accessing care. Addressing these challenges is crucial for the successful integration of telemedicine into rural healthcare systems.
To tackle these issues, healthcare providers and policymakers must work collaboratively to enhance infrastructure and provide education on using telehealth platforms. Initiatives could include:
- Investing in broadband internet access to ensure all communities can connect.
- Offering training programs that help patients navigate telemedicine technologies.
- Creating partnerships with local organizations to promote telehealth services and raise awareness about available resources.
In conclusion, telemedicine holds great promise for transforming healthcare in rural and underserved areas. By breaking down geographical barriers, it not only enhances access to care but also empowers patients to take charge of their health. As we continue to embrace this digital revolution, it’s vital to ensure that no one is left behind, and that everyone has the opportunity to benefit from the advancements in telehealth.
Q: What is telemedicine?
A: Telemedicine is the use of technology to provide healthcare services remotely, allowing patients to consult with healthcare providers via video calls, phone calls, or messaging.
Q: How does telemedicine benefit rural areas?
A: It improves access to healthcare services, reduces travel burdens, and helps manage chronic conditions more effectively, addressing health disparities in these communities.
Q: What are the challenges of telemedicine in rural areas?
A: Key challenges include limited internet connectivity, technological literacy, and the availability of healthcare professionals.
Q: How can these challenges be addressed?
A: Solutions include investing in broadband infrastructure, offering technology training programs, and forming partnerships with local organizations to promote telehealth services.

Ethical Considerations in Telemedicine
As we dive deeper into the world of telemedicine, it's crucial to address the ethical considerations that arise in this digital healthcare landscape. With the rapid adoption of telehealth services, questions about privacy, consent, and equity are at the forefront of discussions among healthcare professionals, patients, and policymakers alike. Imagine walking into a doctor's office where everything is digital; while it sounds convenient, it also raises eyebrows about how personal information is handled and protected.
One of the most pressing concerns is patient privacy. In traditional healthcare settings, there are established protocols to ensure that patient information remains confidential. However, in the realm of telemedicine, where data is transmitted over the internet, the risk of breaches increases. Healthcare providers must implement robust security measures to safeguard sensitive data, including encryption and secure access controls. Patients should also be educated about the potential risks and the steps taken to mitigate them, fostering a sense of trust in the system.
Another critical aspect is informed consent. In a virtual consultation, how can a provider ensure that a patient fully understands the implications of their treatment? Unlike face-to-face interactions, telemedicine can sometimes lead to misunderstandings. It's essential for healthcare providers to clearly communicate treatment options, potential risks, and the nature of the telehealth service being provided. This not only empowers patients but also ensures that they are making informed decisions about their health.
Equity in access to telemedicine is also a significant concern. While telehealth has the potential to break down barriers to care, it can inadvertently widen the gap for those without adequate technology or internet access. Rural communities and underserved populations may find themselves at a disadvantage. Therefore, it is vital for healthcare systems to develop strategies that promote equitable access to telehealth services. This could involve providing resources such as community internet access points or mobile health units that bring care directly to these populations.
Moreover, ethical dilemmas also extend to the use of artificial intelligence (AI) in telemedicine. As AI becomes more integrated into healthcare, issues regarding algorithmic bias and transparency arise. It's imperative that developers and healthcare providers work together to ensure that AI tools are trained on diverse datasets to avoid perpetuating existing health disparities. The goal should be to enhance patient care without compromising ethical standards.
In conclusion, while telemedicine offers exciting possibilities, it is accompanied by a host of ethical considerations that need to be addressed proactively. By prioritizing patient privacy, ensuring informed consent, promoting equitable access, and navigating the complexities of AI, we can create a telehealth landscape that is not only effective but also ethically sound. The future of healthcare is bright, but it must be grounded in ethical principles to truly benefit all.
- What are the main ethical concerns in telemedicine? The primary concerns include patient privacy, informed consent, equitable access to services, and the ethical use of AI technologies.
- How can patient privacy be ensured in telemedicine? Implementing robust security measures such as encryption, secure access controls, and educating patients about data protection can help safeguard privacy.
- What does informed consent look like in a telehealth setting? Informed consent in telehealth requires clear communication from healthcare providers about treatment options, risks, and the nature of the telehealth service.
- How can we promote equity in telemedicine? Strategies such as providing community internet access points and mobile health units can help ensure underserved populations have access to telehealth services.

Future Trends in Telemedicine
The future of telemedicine is not just bright; it’s practically glowing with possibilities! As we look ahead, several exciting trends are shaping the landscape of healthcare delivery. One of the most significant advancements is the integration of artificial intelligence (AI) into telemedicine platforms. Imagine having a virtual assistant that can analyze your health data in real-time, provide personalized recommendations, and even alert healthcare providers if something seems off. This isn’t just a dream; it’s happening now, and it’s set to revolutionize patient care.
Another trend to watch is the rise of personalized medicine. With telemedicine, healthcare can be tailored to fit individual needs more effectively than ever before. Through genetic testing and data analytics, doctors can create customized treatment plans that consider a patient’s unique genetic makeup, lifestyle, and preferences. This means that patients will not only receive care that is more effective but also more aligned with their personal health goals.
Moreover, the evolution of remote patient monitoring technologies is poised to change the game. Devices like smartwatches and health trackers are becoming more sophisticated, allowing for continuous monitoring of vital signs and health metrics. This data can be shared instantly with healthcare providers, enabling proactive interventions. Imagine a world where your doctor can monitor your heart rate or blood sugar levels in real time, adjusting your treatment plan on-the-fly based on live data. This kind of immediate feedback loop could significantly improve health outcomes.
Furthermore, the expansion of telehealth platforms is likely to continue, making healthcare more accessible than ever. With the ability to connect with specialists from anywhere in the world, patients will no longer be limited by geography. This is particularly important for individuals living in rural or underserved areas, who may have previously faced barriers to accessing quality healthcare.
However, as we embrace these advancements, it's crucial to consider the ethical implications that come with them. Issues surrounding data privacy, consent, and equity must be addressed to ensure that telemedicine benefits everyone fairly. The healthcare community must work together to establish guidelines that protect patient information while promoting innovation.
In summary, the future of telemedicine is a tapestry woven with technology, personalization, and accessibility. As we move forward, these trends will not only enhance patient care but also transform the entire healthcare system into a more efficient, responsive, and patient-centered environment. The question is, are we ready to embrace this change?
- What role does AI play in telemedicine? AI can analyze patient data, provide recommendations, and help healthcare providers make informed decisions.
- How does personalized medicine improve patient care? It tailors treatments based on individual genetic and lifestyle factors, leading to more effective healthcare solutions.
- What are remote patient monitoring technologies? These are devices that continuously track health metrics, allowing for real-time data sharing with healthcare providers.
- Can telemedicine improve access to healthcare? Yes, especially for those in rural or underserved areas, by connecting patients with specialists regardless of location.

Telemedicine's Role in Scientific Research
Telemedicine is not just reshaping how patients receive care; it is also making significant strides in the realm of scientific research. Imagine a world where researchers can gather data from participants located in remote areas without the need for them to travel long distances. This is becoming a reality, thanks to telehealth technologies. By leveraging telemedicine, researchers can enhance their studies, recruit diverse participant pools, and collect data in real-time, thereby accelerating the pace of scientific discovery.
One of the most exciting aspects of telemedicine in research is its ability to reach underserved populations. Traditionally, clinical trials have been criticized for their lack of representation, often excluding individuals from rural or low-income backgrounds. However, with telemedicine, researchers can conduct studies that are more inclusive, allowing for a broader understanding of how different demographics respond to treatments. This shift not only improves the quality of research but also ensures that findings are applicable to a wider audience.
Furthermore, telemedicine facilitates the collection of high-quality data. Researchers can utilize various digital tools, such as wearables and mobile apps, to monitor participants' health metrics continuously. This real-time data collection can lead to more accurate results, as it captures fluctuations in health status that might be missed in traditional study designs. For example, a study on heart disease might benefit from continuous heart rate monitoring via a wearable device, providing insights that were previously unattainable.
In addition to improving data collection, telemedicine fosters collaboration among researchers. Virtual platforms enable scientists from different geographical locations to work together seamlessly. This collaborative approach can lead to innovative solutions and shared knowledge, ultimately enhancing the quality of research outcomes. With the ability to conduct virtual meetings and share data instantly, the barriers that once hindered collaboration are rapidly disappearing.
However, the integration of telemedicine into scientific research is not without its challenges. Issues such as data privacy, security, and regulatory compliance must be addressed to ensure that studies are conducted ethically and responsibly. Researchers must navigate the complexities of obtaining informed consent in a virtual environment, which can differ significantly from traditional methods.
As we look to the future, the potential for telemedicine to transform scientific research is immense. With ongoing advancements in technology and a growing understanding of its benefits, we can anticipate an era where telehealth becomes an integral part of research methodologies. This evolution will not only enhance the efficiency of studies but also contribute to more equitable healthcare solutions for all.
- How does telemedicine improve patient recruitment for studies? Telemedicine allows researchers to reach a broader demographic, including those in remote areas, making it easier to recruit diverse participants.
- What are the main ethical concerns related to telemedicine in research? Key concerns include data privacy, informed consent, and ensuring equitable access to participation in studies.
- Can telemedicine lead to better data quality in research? Yes, by enabling continuous monitoring through wearables and apps, researchers can collect more accurate and comprehensive data.
- What role does technology play in facilitating collaboration among researchers? Virtual platforms and tools allow researchers from different locations to share data and insights, improving collaboration and innovation.
Frequently Asked Questions
- What is telemedicine?
Telemedicine refers to the use of technology to provide medical care remotely. It allows healthcare providers to consult with patients via video calls, phone calls, or messaging, making healthcare more accessible and convenient.
- How does telemedicine improve patient care?
Telemedicine enhances patient care by offering timely access to healthcare professionals, reducing the need for travel, and allowing for continuous monitoring of patients through wearable devices. This leads to better health outcomes and more personalized care.
- What technologies are driving telemedicine?
Emerging technologies such as artificial intelligence, telehealth platforms, and wearable health devices are revolutionizing telemedicine. These innovations streamline processes and enable real-time data collection and analysis, improving patient management.
- What challenges does telemedicine face?
Telemedicine faces several challenges, including regulatory hurdles, technological barriers, and issues related to reimbursement. Addressing these challenges is crucial for broader adoption and integration into healthcare systems.
- How does telemedicine affect patient-provider relationships?
Telemedicine changes traditional dynamics by facilitating virtual consultations. While it can enhance accessibility, it’s essential to maintain effective communication and trust through regular follow-ups and personalized care approaches.
- Can telemedicine help underserved communities?
Absolutely! Telemedicine significantly improves access to healthcare in rural and underserved areas, reducing travel burdens and helping to address health disparities by connecting patients with necessary medical resources.
- What ethical considerations are involved in telemedicine?
As telemedicine expands, ethical dilemmas such as privacy, informed consent, and equitable access arise. It’s essential for healthcare providers to navigate these issues responsibly to ensure fair telehealth practices.
- What does the future hold for telemedicine?
The future of telemedicine looks promising, with advancements in AI, personalized medicine, and remote patient monitoring technologies on the horizon. These trends will likely enhance the efficiency and effectiveness of telehealth services.
- How does telemedicine contribute to scientific research?
Telemedicine facilitates scientific research by enabling efficient data collection, patient recruitment, and collaboration among researchers. It allows for larger and more diverse study populations, enhancing the quality of research outcomes.