How New Discoveries are Shaping Neurosurgery
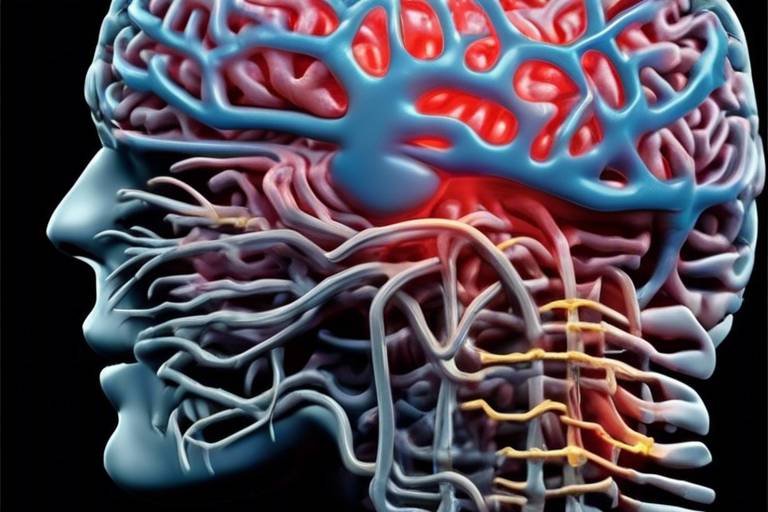
In the ever-evolving field of medicine, neurosurgery stands out as a beacon of innovation and hope. Recent breakthroughs are not just reshaping the way surgeons operate; they are fundamentally transforming patient outcomes, making once-daunting procedures manageable and recovery times significantly shorter. Imagine a world where complex brain surgeries are performed with the precision of a finely tuned machine, where patients can return to their daily lives faster than ever before. This is not just a dream; it's a reality being shaped by advancements in technology, research, and surgical techniques.
As we delve deeper into this fascinating realm, we will explore the latest advancements that are revolutionizing neurosurgery. From cutting-edge imaging techniques that allow for better visualization of brain structures to the emergence of minimally invasive surgical methods that reduce trauma and speed up recovery, each development brings with it a wave of optimism. Neurosurgeons are now equipped with tools and insights that enhance their capabilities, allowing them to tackle challenges with newfound confidence.
Moreover, the integration of robotic-assisted surgery is another game-changer, offering unprecedented precision and control during complex procedures. This technology not only improves surgical outcomes but also enhances patient safety, ensuring that even the most intricate operations can be performed with minimal risk. As we navigate through this article, we'll uncover how these advancements are not just theoretical but are being actively implemented in surgical practices today.
In addition to surgical techniques, we're witnessing a surge in research focused on neuroplasticity and rehabilitation strategies. Understanding how the brain adapts and heals post-surgery is crucial for developing effective recovery protocols. This knowledge empowers healthcare providers to tailor rehabilitation plans that align with each patient's unique needs, promoting a smoother recovery journey.
Finally, the exploration of innovative drug delivery methods is paving the way for more effective treatments for neurological conditions. From targeted therapies that hone in on specific ailments to the groundbreaking use of nanotechnology in drug delivery systems, these advancements are opening new avenues for patient care. As we uncover these layers of innovation, it becomes clear that the future of neurosurgery is not only bright but also filled with possibilities that were once thought to be beyond reach.
- What are the latest advancements in neurosurgery? Recent advancements include improved imaging techniques, robotic-assisted surgeries, and innovative drug delivery methods.
- How do minimally invasive techniques benefit patients? They reduce recovery times, minimize complications, and allow for quicker return to daily activities.
- What role does neuroplasticity play in recovery? Understanding neuroplasticity helps develop effective rehabilitation strategies tailored to individual patient needs.
- How is nanotechnology used in neurosurgery? Nanotechnology enhances drug delivery systems, making treatments more effective and safer for neurological disorders.

Advancements in Imaging Techniques
In the ever-evolving field of neurosurgery, imaging techniques play a pivotal role in enhancing surgical outcomes. Recent advancements in technologies such as Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans have significantly transformed the way neurosurgeons visualize brain structures. These innovations not only aid in more accurate diagnoses but also facilitate meticulous surgical planning, leading to improved patient safety and outcomes.
One of the most exciting developments is the introduction of high-resolution imaging, which allows for a detailed view of the brain's anatomy. This level of detail is crucial, especially when dealing with complex conditions such as tumors or vascular malformations. For instance, advanced MRI techniques, like functional MRI (fMRI), enable surgeons to map brain activity in real-time, ensuring that critical areas responsible for essential functions like speech and movement are preserved during surgery.
Moreover, the integration of 3D imaging has revolutionized pre-surgical planning. Neurosurgeons can now create three-dimensional models of a patient's brain, which helps them visualize the precise location of a tumor or other abnormalities. This technology not only enhances the understanding of the patient's unique anatomy but also allows for better simulation of surgical maneuvers before entering the operating room.
Additionally, the use of intraoperative imaging has become more prevalent. This technique provides real-time images during surgery, allowing surgeons to make immediate adjustments based on what they see. For example, intraoperative CT scans can confirm the removal of a tumor or the successful placement of a device, reducing the likelihood of complications and the need for follow-up surgeries.
These advancements in imaging techniques are not just about improving the surgical process; they also contribute to better patient outcomes. Studies have shown that patients who undergo surgeries with the aid of advanced imaging technologies experience shorter recovery times and fewer complications. This can be attributed to the increased precision in identifying and treating the problem areas while minimizing damage to surrounding healthy tissues.
In summary, the advancements in imaging techniques are reshaping the landscape of neurosurgery. With tools that allow for enhanced visualization, real-time feedback, and detailed anatomical mapping, neurosurgeons are better equipped than ever to tackle complex brain conditions. As these technologies continue to evolve, we can expect even more remarkable improvements in patient care and surgical efficacy.

Minimally Invasive Surgical Techniques
In recent years, have emerged as a game-changer in the field of neurosurgery. These innovative approaches are designed to perform complex procedures while significantly reducing the trauma associated with traditional open surgeries. Imagine a world where patients can undergo brain surgery with just a few small incisions, leading to quicker recoveries and less pain. Sounds like science fiction? Well, it’s becoming a reality!
One of the most significant advantages of minimally invasive techniques is the reduction in recovery time. Patients who undergo these procedures often find themselves back on their feet much sooner than those who have experienced traditional surgeries. This is not just beneficial for the patient’s physical health; it also impacts their emotional well-being. After all, who wouldn’t prefer to spend less time in recovery and more time enjoying life?
Moreover, these techniques are associated with fewer complications and lower rates of infection. By operating through smaller incisions, surgeons minimize damage to surrounding tissues. This precision is crucial, especially when dealing with delicate structures in the brain. As a result, the risk of post-surgical complications diminishes significantly, leading to better overall outcomes for patients.
Some of the commonly used minimally invasive techniques in neurosurgery include:
- Endoscopic Surgery: Utilizing a small camera and instruments inserted through tiny openings, surgeons can access the brain with remarkable precision.
- Keyhole Surgery: This technique involves making a small incision, allowing surgeons to operate on the brain with minimal disruption to surrounding tissues.
- Neuroendoscopy: A specialized form of endoscopic surgery that focuses on the brain and spinal cord, providing a clear view of the surgical site.
As we delve deeper into the realm of minimally invasive techniques, we can’t overlook the role of technology. The integration of advanced imaging technologies, such as MRI and CT scans, plays a pivotal role in enhancing the accuracy of these procedures. Surgeons can visualize the brain's anatomy in real-time, allowing them to navigate complex pathways with confidence and precision.
However, despite the numerous benefits, the transition to minimally invasive techniques is not without its challenges. Surgeons require specialized training to master these intricate procedures. It’s not just about having the right tools; it’s about knowing how to use them effectively. This need for advanced training can sometimes slow the adoption of these techniques across various medical institutions.
In conclusion, minimally invasive surgical techniques are revolutionizing the landscape of neurosurgery. With their ability to reduce recovery times, minimize complications, and enhance patient outcomes, these methods are paving the way for a new era in surgical practices. As technology continues to evolve, we can expect even more exciting advancements in the field, ultimately leading to better care for patients.
What are the main benefits of minimally invasive neurosurgery?
The primary benefits include reduced recovery time, less pain, lower risk of infection, and minimal scarring compared to traditional surgery.
Are all neurosurgical procedures suitable for minimally invasive techniques?
Not all procedures can be performed using minimally invasive techniques. The suitability depends on the specific condition and the surgeon's expertise.
How can patients prepare for minimally invasive neurosurgery?
Patients should discuss their medical history with their surgeon, follow pre-operative instructions, and arrange for post-surgery care to ensure a smooth recovery.
What is the recovery time after minimally invasive neurosurgery?
Recovery times vary depending on the procedure and the individual, but many patients can return to normal activities within a few days to weeks.

Robotic-Assisted Surgery
In the realm of neurosurgery, is not just a buzzword; it's a groundbreaking advancement that is reshaping the way surgeons operate. Imagine having a surgical assistant that never tires, maintains perfect precision, and can maneuver in ways the human hand simply cannot. This is the essence of robotic systems in the operating room. These sophisticated machines are designed to assist surgeons during complex procedures, offering enhanced visualization and dexterity that can significantly improve patient outcomes.
One of the most compelling aspects of robotic-assisted surgery is its ability to provide surgeons with a 3D view of the surgical field, which is crucial when navigating the intricate structures of the brain. This enhanced visualization allows for more accurate targeting of tumors or lesions, minimizing damage to surrounding healthy tissue. Furthermore, the robotic arms can execute delicate maneuvers with a level of precision that is often unattainable through traditional methods. This is akin to using a finely-tuned instrument rather than a blunt tool; the difference in outcome can be staggering.
However, the beauty of robotic-assisted surgery lies not only in its precision but also in its minimally invasive nature. Traditional neurosurgery often involves large incisions, leading to extended recovery times and increased risks of complications. In contrast, robotic systems enable surgeons to operate through much smaller openings, which can drastically reduce recovery times for patients. For instance, studies have shown that patients undergoing robotic-assisted surgeries often experience less postoperative pain and shorter hospital stays, which is a win-win for both the patient and the healthcare system.
Despite these advantages, it’s essential to acknowledge that robotic-assisted surgery is not without its challenges. The initial costs of acquiring and maintaining robotic systems can be substantial, often making it a significant investment for hospitals. Additionally, there is a learning curve associated with these technologies. Surgeons must undergo specialized training to become proficient in using robotic systems, which can delay widespread adoption. However, as more healthcare institutions recognize the potential benefits, the hope is that these barriers will gradually diminish.
In summary, robotic-assisted surgery represents a new frontier in neurosurgery, combining technology and surgical expertise to enhance patient care. As these systems continue to evolve and become more integrated into surgical practices, the future looks promising for both surgeons and patients alike. The marriage of robotics and neurosurgery is not just a trend; it’s a revolution that is making waves in the medical community.
- What is robotic-assisted surgery?
Robotic-assisted surgery involves the use of robotic systems to assist surgeons in performing complex procedures with greater precision and control. - What are the benefits of robotic-assisted surgery?
Benefits include enhanced visualization, reduced recovery times, less postoperative pain, and minimized risks of complications. - Are there any downsides to robotic-assisted surgery?
Challenges include high costs of equipment and the need for specialized training for surgeons. - How does robotic-assisted surgery improve patient outcomes?
By allowing for more precise targeting and minimally invasive techniques, robotic-assisted surgery can lead to better surgical results and quicker recovery times.

Benefits of Robotics in Neurosurgery
Robotic-assisted surgery is transforming the landscape of neurosurgery, ushering in a new era of precision and safety. Imagine a world where the surgeon's hands are guided not just by their skill but also by advanced technology that enhances every movement. This is not science fiction; it's the reality of modern neurosurgery. The integration of robotics into surgical practices offers numerous benefits that significantly improve patient outcomes and operational efficiency.
One of the most compelling advantages of robotic systems is their ability to provide enhanced visualization. With high-definition cameras and sophisticated imaging techniques, surgeons can see intricate details of the brain and surrounding structures that were previously difficult to visualize. This clarity reduces the likelihood of errors during surgery, allowing for more accurate resections of tumors or other abnormalities. Additionally, the robotic arms can maneuver with such precision that they can operate in tight spaces with minimal disruption to surrounding tissues.
Moreover, the dexterity offered by robotic systems is unparalleled. Traditional surgical techniques often require larger incisions and more invasive approaches, leading to longer recovery times. In contrast, robotic-assisted surgeries can be performed through smaller incisions, which not only minimizes trauma to the patient but also significantly shortens recovery periods. Patients often experience less pain, reduced scarring, and a quicker return to their daily activities. This is particularly beneficial for those who lead active lifestyles or have demanding jobs.
Another notable benefit is the reduction in complications. Studies have shown that surgeries performed with robotic assistance often result in fewer postoperative complications. The precision of robotic systems decreases the chance of damaging critical structures in the brain, thereby lowering the risk of complications such as infections, bleeding, or neurological deficits. This aspect is crucial for neurosurgery, where the stakes are exceptionally high, and even a minor error can have significant consequences.
In addition to these advantages, robotic surgery can also enhance the surgeon's capabilities. With features like motion scaling and tremor filtration, robotic systems allow surgeons to perform complex maneuvers that might be challenging with traditional techniques. This means that even the most intricate procedures can be executed with confidence and skill, leading to better outcomes for patients.
As we look towards the future, the role of robotics in neurosurgery will likely continue to expand. Ongoing advancements in technology promise to refine these systems even further, making them more accessible and effective. The potential for robotic systems to improve surgical training and education is also noteworthy. Surgeons can practice and refine their skills in a simulated environment before performing actual procedures, leading to overall enhancements in surgical proficiency.
In summary, the benefits of robotics in neurosurgery are profound and far-reaching. From enhanced visualization and dexterity to reduced complications and improved outcomes, robotic-assisted surgery is paving the way for a revolution in how neurosurgical procedures are performed. As technology continues to evolve, we can expect even greater advancements that will further transform patient care in this critical field.
- What is robotic-assisted neurosurgery?
Robotic-assisted neurosurgery involves the use of robotic systems to aid surgeons in performing complex brain surgeries with enhanced precision and control. - How does robotic surgery improve patient outcomes?
Robotic surgery enhances visualization, reduces recovery time, minimizes complications, and allows for more precise surgical maneuvers. - Are there risks associated with robotic-assisted surgery?
Like all surgical procedures, there are risks, but studies indicate that robotic-assisted surgeries often have lower complication rates compared to traditional methods. - Is robotic-assisted surgery more expensive?
Yes, the initial costs can be higher due to the technology and training required, but the potential for better outcomes may offset these costs in the long run.

Challenges and Limitations
While the integration of robotic systems into neurosurgery has opened up a world of possibilities, it is not without its . One of the most significant hurdles is the high cost associated with these advanced technologies. Robotic surgical systems can cost millions of dollars, which may not be feasible for many hospitals, especially smaller facilities or those in underserved areas. This financial barrier can limit access to cutting-edge surgical techniques, leaving some patients without the benefits of robotic-assisted procedures.
Moreover, the need for specialized training cannot be overlooked. Surgeons must undergo extensive training to operate these robotic systems effectively. This training is not only time-consuming but can also be expensive, adding to the overall cost of implementing robotic surgery in a clinical setting. As a result, there may be a shortage of qualified surgeons who are proficient in these techniques, which can lead to disparities in patient care.
In addition to financial and training challenges, there are also technical limitations that need to be addressed. For instance, robotic systems can sometimes face issues with connectivity and software malfunctions during surgery, which can pose risks to patient safety. These technical glitches can lead to delays or complications, potentially undermining the very advantages that robotic surgery aims to provide.
Furthermore, there is a learning curve associated with the adoption of robotic systems. Surgeons transitioning from traditional methods to robotic-assisted techniques may initially experience a dip in their performance as they adapt to the new technology. This adjustment period can be stressful for both surgeons and patients, as the outcomes may not be as favorable during the early stages of implementation.
Despite these challenges, the potential benefits of robotic-assisted surgery are substantial. As the technology continues to evolve and improve, it is likely that many of these limitations will be addressed. However, it is crucial for healthcare systems to consider these factors when deciding to integrate robotic systems into their surgical practices.
- What are the main benefits of robotic-assisted surgery?
Robotic-assisted surgery offers enhanced precision, reduced recovery times, and minimized complications compared to traditional surgical methods. - Are there risks associated with robotic surgery?
Yes, like any surgical procedure, robotic surgery carries risks, including potential technical malfunctions and the need for specialized training. - How expensive is robotic surgery?
The costs can vary widely, but robotic surgical systems can be quite expensive, often costing millions of dollars, which may affect accessibility. - Is specialized training required for surgeons?
Yes, surgeons must undergo specific training to operate robotic systems effectively, which can be time-consuming and costly.

Neuroplasticity and Rehabilitation
Understanding neuroplasticity is like discovering a hidden superpower within the brain. This remarkable ability of the brain to reorganize itself by forming new neural connections throughout life is a game-changer, especially in the realm of rehabilitation after neurosurgery. Imagine your brain as a bustling city; when a road is blocked (like after an injury), the city finds alternative routes to keep the traffic flowing. Similarly, neuroplasticity allows the brain to adapt and compensate for lost functions, paving the way for recovery.
In the context of neurosurgery, patients often face challenges such as impaired movement, speech difficulties, or cognitive issues post-operation. However, recent research has shown that with the right rehabilitation strategies, these challenges can be addressed effectively. For instance, therapies that stimulate neuroplasticity can help patients regain lost functions and improve their quality of life. Techniques such as mirror therapy, where patients use a mirror to visualize movement in a non-affected limb, have shown promising results in enhancing motor recovery.
Moreover, the integration of technology into rehabilitation practices is further enhancing outcomes. Virtual reality (VR) and interactive video games are being utilized to create engaging rehabilitation environments that encourage patients to practice movements repetitively. This not only makes therapy more enjoyable but also promotes brain adaptability. The repetitive practice is akin to a musician mastering a new song; the more they practice, the more proficient they become. In the same way, patients practicing movements can strengthen neural pathways, leading to improved recovery.
To truly harness the power of neuroplasticity in rehabilitation, a tailored approach is essential. Each patient's journey is unique, and rehabilitation programs should be customized to meet individual needs. Factors such as age, the type of surgery performed, and pre-existing conditions all play a crucial role in determining the best rehabilitation strategy. Here are some key components that can be included in a personalized rehabilitation plan:
- Assessment: Conduct thorough evaluations to understand the specific deficits and strengths of the patient.
- Goal Setting: Collaborate with patients to set realistic and achievable rehabilitation goals.
- Multidisciplinary Approach: Involve a team of professionals, including physical therapists, occupational therapists, and speech therapists, to address various aspects of recovery.
- Ongoing Monitoring: Regularly assess progress and adjust rehabilitation strategies as needed to ensure optimal recovery.
As we look to the future, research into neuroplasticity continues to evolve, promising even more innovative rehabilitation techniques. Scientists are exploring how different factors, such as diet, exercise, and even mindfulness practices, can enhance neuroplasticity. The potential for recovery is expanding, and with it, the hope for patients who face the daunting challenges of neurosurgery.
In conclusion, neuroplasticity is not just a fascinating concept; it is a vital element in the rehabilitation process after neurosurgery. By understanding and leveraging this incredible ability, healthcare providers can create more effective recovery strategies, ultimately transforming the lives of patients. As we continue to unlock the mysteries of the brain, the future of rehabilitation looks brighter than ever.
- What is neuroplasticity? Neuroplasticity is the brain's ability to reorganize itself by forming new neural connections, which is crucial for recovery after injuries or surgeries.
- How does neuroplasticity aid in rehabilitation? It allows the brain to adapt to changes and compensate for lost functions, enabling patients to regain skills and improve their quality of life.
- What rehabilitation techniques promote neuroplasticity? Techniques such as repetitive practice, mirror therapy, and the use of technology like virtual reality can enhance neuroplasticity and aid recovery.
- Why is a personalized rehabilitation plan important? Each patient's recovery journey is unique, and a tailored approach ensures that their specific needs and challenges are addressed effectively.

Innovative Drug Delivery Methods
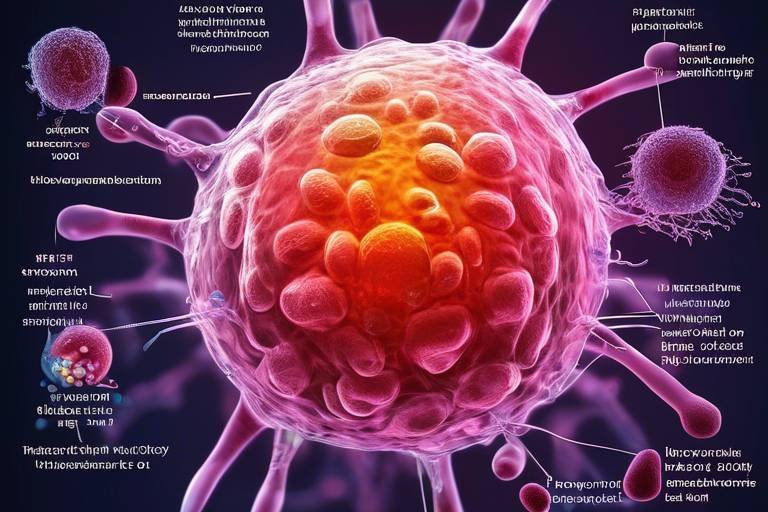
The realm of neurosurgery is undergoing a profound transformation, particularly in how we deliver medications to treat complex neurological conditions. Traditional methods of drug delivery often fall short, leading to ineffective treatment and unnecessary side effects. However, recent innovations are paving the way for more targeted and efficient approaches that promise to enhance patient outcomes significantly. Imagine being able to deliver medication directly to the site of a brain tumor, maximizing efficacy while minimizing systemic side effects—this is not just a dream; it's becoming a reality.
One of the most exciting advancements in this field is the development of targeted drug delivery systems. These systems are designed to concentrate the therapeutic agents precisely where they are needed, ensuring that the maximum amount of the drug reaches the affected area. This is particularly crucial in treating conditions like brain tumors, where traditional systemic therapies often lead to suboptimal results. For instance, researchers are now utilizing liposomal formulations and microbubble technology to enhance the delivery of chemotherapeutic agents directly to tumor sites, significantly improving treatment effectiveness.
Moreover, the advent of nanotechnology has revolutionized the way we think about drug delivery in neurosurgery. Nanoparticles, which are tiny materials measured in nanometers, can be engineered to transport drugs across the blood-brain barrier—a significant hurdle in treating neurological diseases. This capability opens up new avenues for therapies that were previously deemed impossible. For example, using specially designed nanoparticles, researchers can encapsulate drugs and release them in a controlled manner, ensuring that the medication is delivered over an extended period. This not only enhances the therapeutic effect but also reduces the frequency of administration, which is a game changer for patient compliance.
As these innovative drug delivery methods continue to evolve, they also raise critical questions about safety and efficacy. The integration of these technologies into clinical practice requires rigorous testing and validation to ensure that they do not introduce new risks. Nevertheless, the potential benefits are enormous, and ongoing research is likely to yield even more breakthroughs in the near future.
| Drug Delivery Method | Benefits | Applications |
|---|---|---|
| Liposomal Formulations | Enhanced targeting and reduced side effects | Brain tumors, neurodegenerative diseases |
| Microbubble Technology | Improved drug penetration and localized delivery | Localized chemotherapy |
| Nanoparticle Systems | Crosses the blood-brain barrier, controlled release | Various neurological conditions |
In conclusion, the landscape of drug delivery methods in neurosurgery is rapidly changing, driven by technological innovations that enhance the precision and effectiveness of treatments. The integration of these advanced systems not only holds the promise for better patient outcomes but also marks a significant shift in how we approach the treatment of neurological disorders. As we continue to explore the capabilities of targeted therapies and nanotechnology, we can anticipate a future where neurosurgery is not just about the surgery itself but also about delivering the right medication at the right time, tailored specifically for each patient’s unique needs.
- What are targeted drug delivery systems?
Targeted drug delivery systems are designed to deliver medications directly to the site of disease, improving efficacy and minimizing side effects. - How does nanotechnology improve drug delivery?
Nanotechnology allows for the creation of nanoparticles that can cross the blood-brain barrier, enabling more effective treatment of neurological disorders. - What are the benefits of using liposomal formulations?
Liposomal formulations enhance drug targeting and reduce systemic toxicity, making them ideal for treating conditions like brain tumors.

Targeted Therapies
In the ever-evolving landscape of neurosurgery, have emerged as a beacon of hope for patients battling various neurological conditions, particularly brain tumors. Unlike traditional treatments that often take a broad-brush approach, targeted therapies focus on specific molecular targets associated with the disease. This precision not only enhances treatment efficacy but also minimizes collateral damage to healthy tissues, which is a significant concern in neurosurgical practices.
One of the most exciting aspects of targeted therapies is their ability to tailor treatment plans to the individual characteristics of a patient's tumor. For instance, by analyzing the genetic makeup of a tumor, surgeons and oncologists can identify unique mutations that may be driving the cancer's growth. This information allows them to select therapies that specifically inhibit these mutations, leading to a more personalized and effective treatment strategy.
Moreover, the integration of targeted therapies into surgical practices is revolutionizing patient outcomes. For example, drugs like trastuzumab and vemurafenib have shown remarkable success in treating specific types of brain tumors by targeting the HER2 and BRAF pathways, respectively. These advancements highlight the importance of ongoing research and development in the field, as new therapies continue to emerge, offering hope where there was once little.
As these therapies gain traction, it's essential to understand their implications for surgical procedures. Surgeons can now plan operations with a clearer understanding of the tumor's biology, which allows for more precise excisions and better overall outcomes. This shift not only improves survival rates but also enhances the quality of life for patients post-surgery.
Despite the promise of targeted therapies, there are challenges to consider. The complexity of the human genome means that not all tumors will respond to these treatments, and the development of resistance can occur. Therefore, ongoing monitoring and potential adjustments to treatment plans are crucial. Nevertheless, the potential benefits far outweigh the challenges, making targeted therapies a vital component of modern neurosurgical practices.
In summary, the rise of targeted therapies in neurosurgery represents a significant leap forward in the fight against neurological diseases. By focusing on the specific characteristics of tumors, these therapies offer a tailored approach that enhances treatment efficacy while minimizing side effects. As research continues to unveil new molecular targets and therapies, we can expect to see even greater advancements in patient care and outcomes in the realm of neurosurgery.
- What are targeted therapies? Targeted therapies are treatments that specifically attack cancer cells based on their unique molecular characteristics, minimizing damage to healthy cells.
- How do targeted therapies differ from traditional treatments? Unlike traditional treatments, which may affect all rapidly dividing cells, targeted therapies focus on specific pathways or mutations within cancer cells.
- Are targeted therapies effective for all types of brain tumors? While many brain tumors can benefit from targeted therapies, their effectiveness varies depending on the tumor's genetic makeup.
- What are some examples of targeted therapies used in neurosurgery? Drugs like trastuzumab and vemurafenib are examples of targeted therapies that have shown promise in treating specific types of brain tumors.

Nanotechnology in Neurosurgery
Nanotechnology is rapidly emerging as a groundbreaking frontier in the field of neurosurgery, offering innovative solutions that promise to change the way we approach treatment for neurological disorders. Imagine being able to deliver medication directly to the site of a brain tumor, minimizing side effects and maximizing effectiveness. This is not just a fantasy; it’s becoming a reality thanks to the advancements in nanotechnology. By manipulating materials at the molecular level, scientists and surgeons are developing nanoparticles that can traverse the blood-brain barrier, a significant hurdle in treating brain diseases.
One of the most exciting aspects of using nanotechnology in neurosurgery is its ability to create targeted drug delivery systems. These systems can encapsulate drugs within nanoparticles that are specifically designed to release their payload at the precise location where treatment is needed. This targeted approach not only enhances the effectiveness of the drugs but also significantly reduces the risk of systemic side effects. For instance, traditional chemotherapy can wreak havoc on the entire body, but with nanotechnology, the treatment can be localized, sparing healthy tissue and reducing the adverse reactions that patients often face.
Moreover, the versatility of nanotechnology allows for the incorporation of various therapeutic agents, including chemotherapeutic drugs, gene therapies, and even immunotherapies. This opens the door for combination therapies that can tackle complex neurological conditions more effectively. For example, a nanoparticle could be engineered to not only deliver a chemotherapeutic agent but also to carry a gene-editing tool that can modify the genetic expression of cancer cells, thereby attacking the tumor from multiple angles.
Despite the promising potential, the application of nanotechnology in neurosurgery is still in its infancy, and there are several challenges that need to be addressed. Safety is a primary concern; the long-term effects of nanoparticles in the human body are not yet fully understood. Additionally, regulatory hurdles can slow down the process of bringing these innovative treatments to market. Researchers are working diligently to ensure that the nanoparticles are biocompatible and that they do not elicit adverse immune responses.
In conclusion, the future of neurosurgery may well be intertwined with the advancements in nanotechnology. As researchers continue to explore the possibilities and overcome the challenges, we can expect to see a paradigm shift in how neurological disorders are treated. The potential for improved patient outcomes, coupled with reduced side effects, makes nanotechnology a beacon of hope for both patients and healthcare professionals alike.
- What is nanotechnology in neurosurgery? Nanotechnology refers to the manipulation of materials at the molecular level to create innovative drug delivery systems that target specific areas in the brain.
- How does nanotechnology improve drug delivery? It allows for targeted delivery of medications directly to the site of a brain tumor, minimizing side effects and enhancing treatment efficacy.
- Are there any risks associated with nanotechnology? Yes, the long-term effects of nanoparticles in the human body are still being studied, and safety is a primary concern.
- What types of therapies can nanotechnology deliver? Nanotechnology can deliver chemotherapeutic agents, gene therapies, and immunotherapies, offering a multi-faceted approach to treatment.
Frequently Asked Questions
- What are the latest advancements in imaging techniques for neurosurgery?
Recent advancements in imaging technologies, such as high-resolution MRI and advanced CT scans, are revolutionizing how neurosurgeons visualize brain structures. These innovations enhance diagnostic accuracy and improve surgical planning, allowing for more precise interventions.
- How do minimally invasive surgical techniques benefit patients?
Minimally invasive surgical techniques significantly reduce recovery times and minimize complications. By using smaller incisions and advanced tools, patients experience less pain, shorter hospital stays, and quicker returns to their daily activities, making the surgical experience much more comfortable.
- What role does robotic-assisted surgery play in neurosurgery?
Robotic-assisted surgery offers enhanced precision and control during complex procedures. Surgeons can perform intricate tasks with greater accuracy, leading to improved patient outcomes and reduced risks. This technology is changing the landscape of neurosurgery by elevating the standard of care.
- What are the benefits of using robotics in neurosurgery?
Robotic systems provide surgeons with enhanced visualization, greater dexterity, and improved safety during operations. These advantages lead to better surgical results and can significantly enhance the overall patient experience.
- What challenges do robotic systems face in neurosurgery?
Despite their benefits, robotic systems come with high costs and require specialized training for surgeons. These challenges can hinder widespread adoption, making it essential for medical institutions to weigh the pros and cons before investing in this technology.
- How does understanding neuroplasticity influence rehabilitation?
Understanding neuroplasticity is vital for developing effective rehabilitation strategies after neurosurgery. This knowledge helps healthcare providers create tailored recovery protocols that leverage the brain's ability to adapt and heal, ultimately enhancing patient recovery outcomes.
- What are innovative drug delivery methods in neurosurgery?
Innovative drug delivery systems are being developed to target brain tumors and other neurological conditions more effectively. These advancements allow for precise medication delivery, improving treatment efficacy and minimizing side effects for patients.
- How are targeted therapies changing neurosurgery?
Targeted therapies are transforming neurosurgery by offering more effective treatment options tailored to specific conditions. By focusing on the unique characteristics of each patient's condition, these therapies enhance the likelihood of successful outcomes.
- What role does nanotechnology play in neurosurgery?
Nanotechnology is revolutionizing drug delivery systems by enabling the use of nanoparticles to target neurological disorders more effectively. This approach increases treatment efficacy and safety, providing new hope for patients facing challenging conditions.