The Latest Findings on Microbial Resistance to Antibiotics
In recent years, the medical community has been grappling with a growing crisis: microbial resistance to antibiotics. This phenomenon, where bacteria evolve to withstand the effects of medications designed to eliminate them, poses a significant threat to public health. Imagine a world where common infections become untreatable, and minor surgeries carry the risk of life-threatening complications due to resistant bacterial infections. It sounds like a plot from a dystopian novel, but it's becoming an alarming reality.
As we delve into the latest discoveries surrounding this issue, it’s essential to understand that antibiotic resistance is not merely a result of over-prescribing medications. It’s a complex interplay of various factors, including genetic mutations, environmental influences, and human behavior. Recent studies have been shedding light on these intricate mechanisms, revealing insights that could shape our approach to tackling this crisis. For instance, researchers have identified specific genetic mutations that allow bacteria to survive in the presence of antibiotics, and understanding these mutations is crucial for developing new treatment strategies.
Moreover, the implications of antibiotic resistance extend beyond individual health. They ripple through our healthcare systems, affecting everything from hospital stays to the effectiveness of routine procedures. The rise of multi-drug resistant organisms (MDROs) is a pressing concern, and as we explore the latest findings, we must consider the broader impact on global health. It’s a call to action for researchers, healthcare providers, and policymakers alike to collaborate and devise effective strategies to combat this growing threat.
In the sections that follow, we will explore the mechanisms behind antibiotic resistance, recent research insights, and the environmental factors that contribute to this issue. We will also discuss the global health implications and potential strategies for mitigation. Buckle up, because the journey through the world of microbial resistance is as intricate as it is urgent!

Understanding Antibiotic Resistance
Antibiotic resistance is a growing concern in the medical community, and it occurs when bacteria evolve to become immune to the effects of antibiotics. This phenomenon is not just a laboratory curiosity; it has real-world implications that affect the treatment of infections globally. Imagine using a powerful tool to fight off an enemy, only to find that the enemy has developed armor that renders your weapon ineffective. That's precisely what antibiotic resistance does—it transforms once-treatable infections into formidable foes.
The mechanisms behind antibiotic resistance are complex and multifaceted. At its core, this resistance can arise through several pathways, including genetic mutations, which can occur naturally or be induced by the overuse of antibiotics. When antibiotics are used excessively, they create a selective pressure on bacterial populations. This means that only the bacteria that have developed some form of resistance will survive, while the susceptible ones are eliminated. Over time, these resistant strains proliferate, leading to a situation where standard treatments fail.
Moreover, the significance of antibiotic resistance extends beyond individual health. It poses a threat to public health systems, as common procedures and surgeries become riskier due to the potential for untreatable infections. The World Health Organization (WHO) has classified antibiotic resistance as one of the top ten global public health threats facing humanity. This is not just a problem for healthcare providers; it affects everyone, from patients to policymakers.
To further illustrate the impact of antibiotic resistance, consider the following key points:
- Increased Morbidity and Mortality: Infections caused by resistant bacteria can lead to longer hospital stays, higher medical costs, and increased mortality.
- Limited Treatment Options: As resistance grows, the number of effective antibiotics diminishes, forcing healthcare providers to rely on older, less effective, or more toxic medications.
- Spread of Resistance: Resistant bacteria can spread from person to person and even between different species, complicating efforts to control infections.
Understanding antibiotic resistance is crucial for developing effective strategies to combat it. By recognizing how bacteria adapt and survive, we can take proactive measures to preserve the efficacy of existing antibiotics and invest in new research for alternative treatments. The fight against antibiotic resistance is not just a battle for healthcare providers; it's a collective challenge that requires awareness and action from all sectors of society.
Recent Research Insights
Recent studies have unveiled alarming trends in microbial resistance patterns that are shaking the very foundations of modern medicine. As researchers delve deeper into this pressing issue, they are uncovering a complex web of factors contributing to the rise of antibiotic-resistant bacteria. For instance, a pivotal study published in Nature highlighted that resistance rates have surged dramatically in the past decade, with some pathogens showing resistance to multiple drug classes. This trend is not just a statistic; it represents a growing threat to effective treatment options for common infections.
One of the most striking findings is the emergence of superbugs, which are bacteria that have developed resistance to last-resort antibiotics. These superbugs are not just confined to hospitals; they are increasingly found in community settings, complicating treatment for everyday infections. The implications of these findings are profound, as we may soon find ourselves in a situation where routine procedures, such as surgeries or cancer treatments, could become perilous due to the risk of untreatable infections.
Moreover, the research indicates that the patterns of resistance are not uniform. Different regions and environments exhibit varying levels of resistance, influenced by local antibiotic usage and public health policies. For example, a study conducted in Europe revealed that countries with stringent antibiotic regulations had significantly lower rates of resistance compared to those with lax policies. This suggests that strategic interventions could potentially mitigate the spread of resistance.
At the heart of this resistance phenomenon are genetic mutations that allow bacteria to adapt and survive in the presence of antibiotics. These mutations can occur spontaneously or be acquired through various mechanisms, such as horizontal gene transfer. This process enables bacteria to share resistance traits, leading to rapid dissemination of resistant strains. For instance, a recent study found that a single resistant strain of E. coli could spread its resistance genes to other strains within a matter of hours, showcasing the alarming speed at which resistance can proliferate.
Horizontal gene transfer is like a bacterial version of sharing secrets; once one bacterium learns how to resist a certain antibiotic, it can pass that knowledge on to its neighbors. This sharing can occur through several mechanisms, including transformation, transduction, and conjugation. Understanding these processes is crucial for developing strategies to combat antibiotic resistance. Researchers are now investigating ways to disrupt these pathways, potentially hindering the spread of resistance among bacterial populations.
Another critical factor in the resistance landscape is the formation of biofilms. Biofilms are communities of bacteria that adhere to surfaces and create a protective barrier, making them significantly more resistant to antibiotic treatment. These resilient structures can form on medical devices, wounds, and even in our bodies. Research has shown that bacteria within biofilms can be up to 1,000 times more resistant to antibiotics than their free-floating counterparts. This complicates treatment strategies and highlights the need for innovative approaches to tackle infections associated with biofilms.
As we unravel these complex interactions and factors influencing antibiotic resistance, it becomes increasingly clear that a multifaceted approach is necessary. Addressing this issue requires not only understanding the science behind resistance but also implementing effective public health strategies to combat its spread.
- What is antibiotic resistance? Antibiotic resistance occurs when bacteria evolve and become immune to the effects of medications designed to kill them.
- Why is antibiotic resistance a concern? It poses a serious threat to public health, making infections harder to treat and increasing the risk of disease spread, severe illness, and death.
- How can we combat antibiotic resistance? Strategies include improved antibiotic stewardship, increased surveillance, and public awareness campaigns.
The Role of Genetic Factors
When we dive into the world of antibiotic resistance, one of the most fascinating yet concerning aspects is the role of genetic factors. Bacteria, much like us, have their own unique DNA that dictates how they function and survive. Over time, some of these microorganisms have developed genetic mutations that allow them to withstand the effects of antibiotics, turning what was once a reliable treatment option into a mere suggestion. Imagine a superhero gaining the power to resist every attack; that's essentially what happens with these bacteria.
These genetic mutations can occur through various mechanisms, such as spontaneous mutations during DNA replication or as a result of exposure to antibiotics. When bacteria are exposed to these drugs, those with a genetic mutation that confers resistance are more likely to survive and reproduce. This leads to a population that is increasingly resistant to treatment. To put it into perspective, consider a group of people trying to climb a mountain. If a few have specially designed climbing gear (the mutations), they will make it to the top, while the others struggle and fall behind. Over time, the mountain becomes populated with climbers who all have that gear—making it harder for anyone without it to succeed.
Moreover, the genetic factors that contribute to antibiotic resistance are not isolated. They can be shared among bacteria through a process known as horizontal gene transfer. This is where things get particularly interesting. Bacteria can exchange genetic material, allowing them to share resistance traits with one another. It's like a secret handshake that grants access to a special club of invincible bacteria. This process can occur in various ways, including:
- Transformation: Bacteria can take up free-floating DNA from their environment.
- Conjugation: Bacteria can transfer DNA directly through physical contact.
- Transduction: Viruses can carry DNA from one bacterium to another.
These mechanisms of gene transfer mean that a single resistant bacterium can quickly lead to a population of resistant bacteria, making it incredibly challenging to control infections. Additionally, some bacteria form biofilms, which are structured communities of bacteria that adhere to surfaces. Within these biofilms, genetic exchange can occur at an accelerated rate, further complicating treatment strategies.
Understanding the role of genetic factors in antibiotic resistance is crucial for developing effective strategies to combat this growing threat. As researchers continue to unravel the complexities of bacterial genetics, we gain invaluable insights into how to outsmart these resilient foes. It's a race against time, and the more we know, the better equipped we are to preserve the effectiveness of antibiotics for future generations.
Horizontal Gene Transfer
Horizontal gene transfer (HGT) is a fascinating and intricate process that allows bacteria to exchange genetic material with one another, rather than passing it down through traditional reproduction. Imagine a bustling city where neighbors share tools and resources, enhancing their own capabilities and making them more resilient. In the bacterial world, this sharing can lead to the rapid spread of antibiotic resistance, making it a significant concern for public health.
One of the most alarming aspects of HGT is its efficiency. Bacteria can acquire resistance genes from other bacteria in their vicinity, even if they are from different species. This capability acts like a shortcut in evolution, allowing resistant traits to spread at an astonishing pace. For instance, if one bacterium develops a mutation that makes it resistant to a specific antibiotic, it can share that trait with its neighbors through several mechanisms, including transformation, transduction, and conjugation.
To break it down further:
- Transformation: This occurs when bacteria take up free-floating DNA from their environment. If that DNA contains resistance genes, the recipient bacterium can incorporate these genes into its own genome.
- Transduction: In this process, bacteriophages (viruses that infect bacteria) can accidentally carry resistance genes from one bacterium to another during infection, effectively acting as a delivery system for these traits.
- Conjugation: This is a direct transfer of DNA between two bacteria that are temporarily joined together. Think of it as a handshake where one bacterium passes a plasmid (a small DNA molecule) containing resistance genes to its partner.
The implications of HGT are profound. It not only accelerates the spread of antibiotic resistance but also complicates treatment options for infections. When bacteria can easily share resistance traits, the effectiveness of existing antibiotics diminishes, leading to longer hospital stays, higher medical costs, and increased mortality rates. The ability of bacteria to adapt and evolve in this way is akin to a game of whack-a-mole; just when we think we've managed to control one strain, another resistant strain pops up somewhere else.
Moreover, HGT is not limited to clinical settings. Environmental factors, such as the use of antibiotics in agriculture and the presence of antibiotics in wastewater, can create hotspots for resistance development. In these environments, bacteria can thrive and exchange resistance genes, which can eventually make their way into human populations. This interconnectedness underscores the importance of a One Health approach, recognizing that human, animal, and environmental health are all linked.
In summary, horizontal gene transfer is a critical mechanism that enhances the spread of antibiotic resistance among bacteria. Understanding how this process works is essential for developing effective strategies to combat the growing threat of resistant infections. As we continue to research and uncover the complexities of microbial resistance, we must remain vigilant and proactive in our efforts to safeguard public health.
- What is horizontal gene transfer?
Horizontal gene transfer is the process by which bacteria exchange genetic material with one another, allowing for the rapid spread of traits such as antibiotic resistance. - How does horizontal gene transfer contribute to antibiotic resistance?
HGT allows resistant bacteria to share their resistance genes with neighboring bacteria, making it easier for non-resistant strains to become resistant. - What are the mechanisms of horizontal gene transfer?
The three main mechanisms are transformation, transduction, and conjugation, each facilitating the exchange of genetic material in different ways. - Why is understanding horizontal gene transfer important?
Understanding HGT is crucial for developing effective strategies to combat antibiotic resistance and protect public health.

Impact of Biofilms
Biofilms are fascinating yet troublesome structures formed by communities of bacteria that adhere to surfaces, both biotic and abiotic. Imagine a city where each building is a bacteria, and together they create a resilient fortress. This is precisely what biofilms do—they provide a protective barrier that makes it significantly harder for antibiotics and the immune system to penetrate and eliminate the bacteria within. In fact, studies suggest that bacteria in biofilms can be up to 1,000 times more resistant to antibiotics than their free-floating counterparts. This incredible resilience is a major hurdle in treating persistent infections.
Biofilms can develop on a variety of surfaces, including medical devices like catheters and implants, as well as natural surfaces such as teeth, leading to conditions like dental plaque. Once established, these biofilms can be incredibly difficult to eradicate, leading to chronic infections that can linger for months or even years. The complexity of biofilms is not just in their physical structure but also in the way they communicate with each other. Bacteria within a biofilm can share resources and even genetic material, enhancing their survival capabilities. This phenomenon is known as quorum sensing, where bacteria release signaling molecules to coordinate their behavior as a collective unit.
The presence of biofilms in clinical settings poses significant challenges for treatment. For instance, when a patient has a prosthetic joint or heart valve, the risk of biofilm formation increases dramatically. Once a biofilm is established on such devices, standard antibiotic treatments often fail, leading to complications that may require surgical intervention to remove the infected device. This not only complicates the treatment process but also increases healthcare costs and the duration of patient suffering.
Moreover, biofilms are not just a problem in healthcare; they are also prevalent in agricultural settings and natural environments. For example, biofilms can form on crops, leading to reduced yield and increased susceptibility to diseases. In water systems, biofilms can create issues with water quality and infrastructure, leading to costly repairs and maintenance. The environmental and economic impacts of biofilms are vast, underscoring the need for innovative strategies to combat them.
In summary, the impact of biofilms on antibiotic resistance is profound and multifaceted. They not only complicate treatment regimens but also contribute to the broader issue of antimicrobial resistance. Understanding the behavior and characteristics of biofilms is crucial for developing effective strategies to combat their effects, whether in clinical settings or in the environment.
- What are biofilms? Biofilms are communities of bacteria that adhere to surfaces and are encased in a protective matrix, making them resistant to antibiotics.
- Why are biofilms a problem in healthcare? They can lead to persistent infections, complicate treatment, and increase healthcare costs.
- How can we combat biofilms? Strategies include improving cleaning protocols, using antimicrobial coatings on medical devices, and developing new therapies that target biofilms specifically.
- Can biofilms form in nature? Yes, biofilms can form on natural surfaces, such as rocks in rivers, and can impact ecosystems and agriculture.
Environmental Influences on Resistance
The environment plays a pivotal role in the development and spread of antibiotic resistance. It's not just about how we use antibiotics in healthcare settings; it's about the larger ecosystem in which these bacteria live. Various environmental factors contribute to the emergence of resistant strains, and understanding these influences is crucial in tackling the issue effectively.
One of the primary contributors is pollution. Industrial waste, agricultural runoff, and improper disposal of pharmaceuticals introduce antibiotics and resistant bacteria into our water systems and soil. This creates a perfect breeding ground for bacteria to adapt and evolve. For instance, when antibiotics are present in the environment, they exert selective pressure on bacterial populations, allowing only those that have developed some form of resistance to survive and thrive. Over time, these resistant bacteria can multiply, leading to a higher prevalence of antibiotic-resistant infections.
Furthermore, agricultural practices significantly impact microbial resistance. The use of antibiotics in livestock is a common practice aimed at preventing disease and promoting growth. However, this practice can lead to the development of resistant bacteria that can transfer to humans through the food chain. In fact, studies have shown that antibiotic-resistant bacteria can be found in the meat we consume, posing a direct threat to public health.
Another environmental factor is waste management. Inadequate sewage treatment can result in the release of untreated or partially treated wastewater into natural water bodies. This not only contaminates the water supply but also facilitates the spread of antibiotic-resistant bacteria. When these bacteria enter our ecosystems, they can interact with other microbial communities, further enhancing their resistance capabilities.
To illustrate the interconnectedness of these factors, consider the following table, which summarizes the main environmental influences on antibiotic resistance:
| Environmental Factor | Impact on Antibiotic Resistance |
|---|---|
| Pollution | Introduction of antibiotics into ecosystems leads to selective pressure on bacteria. |
| Agricultural Practices | Use of antibiotics in livestock promotes the development of resistant strains. |
| Waste Management | Inadequate sewage treatment spreads resistant bacteria into natural water bodies. |
Moreover, urbanization and population density also play a role in the spread of resistance. As cities grow, the concentration of people and waste increases, creating environments where resistant bacteria can spread more easily. It's a vicious cycle: the more we encroach on natural habitats, the more we disrupt the balance of microbial communities, leading to increased resistance.
In conclusion, environmental influences on antibiotic resistance are complex and multifaceted. Addressing these factors requires a concerted effort from policymakers, healthcare providers, and the general public. By understanding the environmental context of antibiotic resistance, we can develop more effective strategies to combat this growing threat.
- What is antibiotic resistance? Antibiotic resistance occurs when bacteria evolve and become immune to the effects of medications designed to kill them.
- How does pollution contribute to antibiotic resistance? Pollution introduces antibiotics into the environment, creating selective pressure that allows resistant bacteria to survive and multiply.
- What role does agriculture play in antibiotic resistance? The use of antibiotics in livestock can lead to the development of resistant bacteria that can transfer to humans through the food chain.
- How can we combat antibiotic resistance? Strategies include improving waste management, regulating antibiotic use in agriculture, and increasing public awareness about the issue.

Global Health Implications
The rise of antibiotic-resistant bacteria is not just a concern for the medical community; it poses a **serious threat** to global health systems. As these resistant strains proliferate, they become increasingly difficult to treat, leading to longer hospital stays, higher medical costs, and an increased risk of mortality. Imagine a world where minor infections, once easily treatable, could become life-threatening due to the ineffectiveness of antibiotics. This scenario is becoming a reality, and the implications are dire.
One of the most alarming aspects of antibiotic resistance is its **impact on public health**. Infections that were once manageable are now causing complications that can lead to severe health crises. For instance, surgeries that rely on antibiotics to prevent infections become riskier, and treatments for chronic diseases can be compromised. This situation can lead to a vicious cycle where the healthcare system is overwhelmed, and patients face dire outcomes.
Furthermore, the economic burden of antibiotic resistance is staggering. It is estimated that the **annual costs** associated with antibiotic-resistant infections in the U.S. alone could exceed **$20 billion** in direct healthcare expenses, not to mention the indirect costs associated with lost productivity and prolonged illness. This financial strain affects not only individual patients but also healthcare providers and insurers, ultimately trickling down to taxpayers. The table below outlines the projected costs associated with antibiotic resistance:
| Cost Category | Estimated Annual Cost (USD) |
|---|---|
| Direct Healthcare Costs | $20 billion |
| Lost Productivity | $35 billion |
| Total Economic Impact | $55 billion |
As we delve deeper into this issue, it becomes evident that **urgent action** is needed. The implications of antibiotic resistance extend beyond individual health; they threaten to undermine the very foundations of modern medicine. Governments, healthcare providers, and pharmaceutical companies must collaborate to develop new antibiotics, implement effective stewardship programs, and enhance public awareness regarding the responsible use of antibiotics.
Moreover, it’s crucial to recognize that antibiotic resistance is a **global issue** that requires a unified response. Countries across the globe must work together to monitor resistance patterns, share data, and develop strategies that can be implemented at both local and international levels. This collaborative effort can help to mitigate the impact of antibiotic-resistant bacteria and protect public health for future generations.
In conclusion, the implications of antibiotic resistance are profound and multifaceted. It is a challenge that demands immediate attention and action. By understanding the gravity of the situation and working collectively, we can combat this growing threat and safeguard the health of populations worldwide.
- What is antibiotic resistance? Antibiotic resistance occurs when bacteria evolve and become immune to the effects of antibiotics, making infections harder to treat.
- Why is antibiotic resistance a global health issue? It affects healthcare systems worldwide, leading to longer hospital stays, increased healthcare costs, and higher mortality rates.
- What can be done to combat antibiotic resistance? Strategies include improving antibiotic stewardship, enhancing surveillance, and increasing public awareness about responsible antibiotic use.

Healthcare Costs and Burden
The economic implications of antibiotic resistance are staggering and demand our immediate attention. As bacteria evolve and become resistant to existing treatments, healthcare systems face mounting pressures that translate into significant financial burdens. This phenomenon not only affects hospitals and clinics but also extends to public health systems, insurance providers, and ultimately, the taxpayers. Let's break down some of the key factors contributing to these soaring costs.
First and foremost, the rise of antibiotic-resistant infections leads to longer hospital stays. Patients with resistant infections often require more intensive care, which increases the time they spend in medical facilities. Studies indicate that patients suffering from these infections can stay in the hospital up to twice as long as those with non-resistant strains. This extended duration not only strains healthcare resources but also escalates treatment costs dramatically.
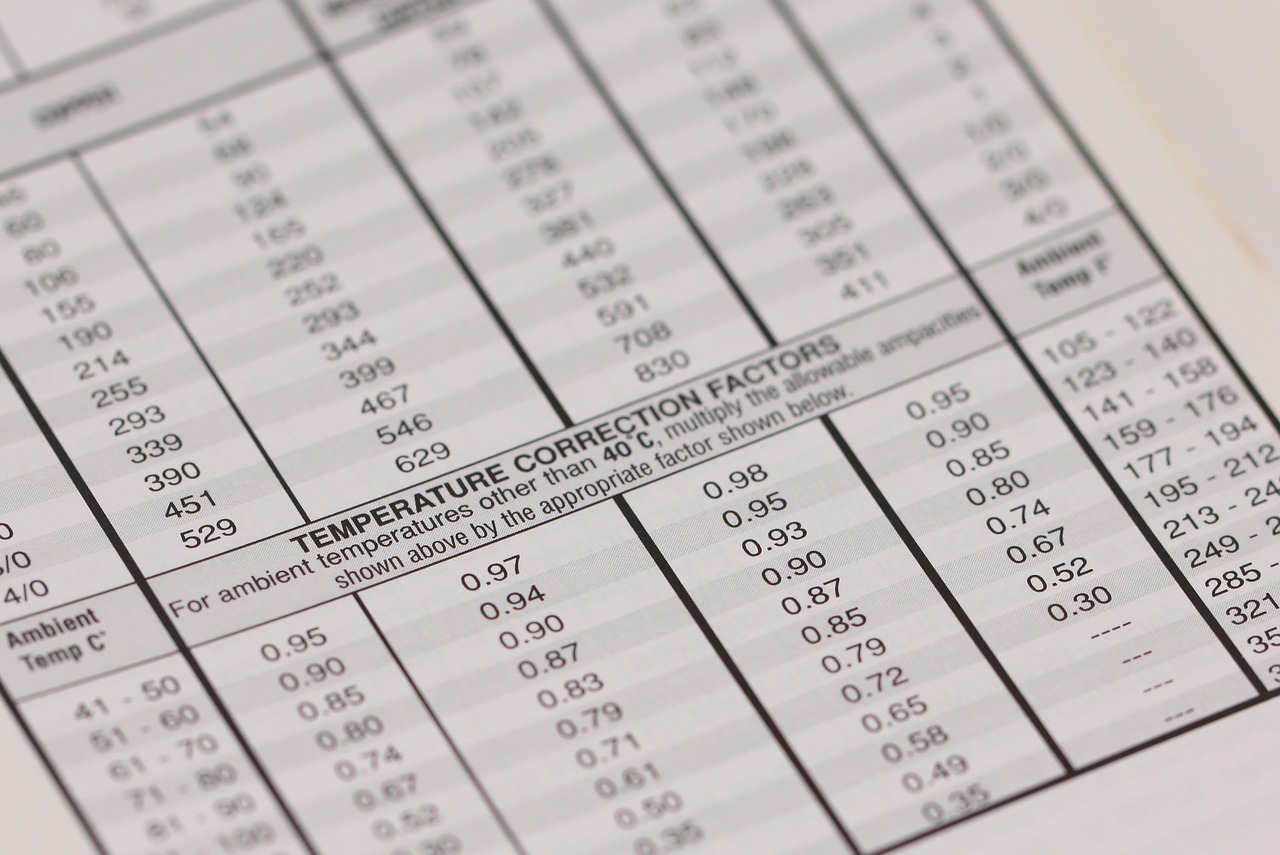
Moreover, the cost of alternative treatments can be exorbitant. As resistance to first-line antibiotics grows, healthcare providers are compelled to use more expensive and often less effective second-line or third-line treatments. This shift not only impacts the financial aspect of healthcare but also raises concerns about patient outcomes. The table below illustrates the comparative costs associated with different treatment options:
| Antibiotic Type | Cost per Treatment | Effectiveness |
|---|---|---|
| First-line Antibiotics | $10 - $50 | High |
| Second-line Antibiotics | $100 - $300 | Moderate |
| Third-line Antibiotics | $500+ | Variable |
In addition to treatment costs, there are indirect costs to consider, such as lost productivity. When individuals fall ill due to antibiotic-resistant infections, they may miss work or school, leading to a ripple effect that impacts the economy. The World Health Organization estimates that the economic burden of antibiotic resistance could reach trillions of dollars globally if not addressed effectively.
Furthermore, the burden on healthcare systems isn't just financial; it also affects the quality of care. With resources stretched thin, healthcare providers may find it challenging to maintain high standards of treatment, leading to poorer patient outcomes. This cycle of resistance and economic strain is a pressing issue that requires immediate and collective action.
In conclusion, the healthcare costs associated with antibiotic resistance are not just numbers on a balance sheet; they represent real challenges that affect patient care, public health, and the economy. Addressing this crisis is imperative, and it requires a concerted effort from healthcare providers, policymakers, and the public to mitigate the burden of antibiotic resistance.
- What is antibiotic resistance? Antibiotic resistance occurs when bacteria evolve and become immune to the effects of antibiotics, making infections harder to treat.
- How does antibiotic resistance impact healthcare costs? It leads to longer hospital stays, the use of more expensive treatments, and lost productivity, all of which contribute to higher healthcare costs.
- What can be done to combat antibiotic resistance? Strategies include improved surveillance, antibiotic stewardship programs, and public awareness campaigns to educate people about responsible antibiotic use.

Strategies for Mitigation
Addressing the issue of antibiotic resistance is no small feat; it requires a concerted effort from healthcare professionals, policymakers, and the general public. The complexity of this problem means that a single solution won't cut it. Instead, we need a multifaceted approach that incorporates various strategies to tackle this growing threat effectively. So, what can we do? Let's dive into some of the most promising strategies for mitigating antibiotic resistance.
First and foremost, improved surveillance of antibiotic use and resistance patterns is crucial. By monitoring how antibiotics are prescribed and how bacteria respond, we can identify trends and intervene before they escalate. This involves not just hospitals but also outpatient settings and agricultural practices where antibiotics are frequently used. For example, countries that have implemented robust surveillance systems have seen a reduction in antibiotic-resistant infections. Isn't it fascinating how data can be a game-changer in this battle?
Another vital strategy is the implementation of antibiotic stewardship programs. These programs aim to promote the appropriate use of antibiotics, ensuring that they are prescribed only when necessary and that the right drug, dose, and duration are chosen. Healthcare facilities can benefit immensely from these programs by reducing unnecessary prescriptions and, consequently, the development of resistance. Think of it as a responsible diet for bacteria—just like we should be mindful of what we eat, we must also be careful about what we give to bacteria.
Public awareness campaigns play a significant role in educating the community about the dangers of antibiotic misuse. We often hear about the importance of completing a prescribed course of antibiotics, but how often do we discuss the consequences of self-medication or using leftover antibiotics? Engaging the public through educational initiatives can empower individuals to make informed decisions, ultimately leading to a decrease in resistance rates. Imagine a world where patients understand that antibiotics are not a cure-all and that their misuse could have dire consequences—not just for them but for everyone.
Moreover, we should not overlook the importance of investing in research and development of new antibiotics and alternative therapies. The pharmaceutical industry has been hesitant to invest in antibiotic development due to the lower profit margins compared to chronic disease treatments. However, innovative funding models and public-private partnerships can incentivize research in this area. Just as we need new cars to replace old, inefficient models, we need new antibiotics to stay ahead of evolving bacteria.
Finally, we must address the environmental factors contributing to antibiotic resistance. Pollution, especially from pharmaceutical waste and agricultural runoff, can lead to the proliferation of resistant bacteria in our ecosystems. Implementing stricter regulations on waste management and promoting sustainable agricultural practices can help mitigate this issue. Think of the environment as a garden; if we don't take care of it, weeds (in this case, resistant bacteria) will flourish.
In summary, the fight against antibiotic resistance is a shared responsibility. By embracing a combination of improved surveillance, antibiotic stewardship, public education, investment in research, and environmental protection, we can make significant strides in mitigating this pressing issue. The path ahead may be challenging, but with collective action, we can pave the way for a healthier future.
- What is antibiotic resistance?
Antibiotic resistance occurs when bacteria evolve and become immune to the effects of medications designed to kill them. - Why is antibiotic resistance a global concern?
The rise of antibiotic-resistant bacteria poses serious threats to public health, making infections harder to treat and increasing healthcare costs. - How can I help combat antibiotic resistance?
You can help by using antibiotics responsibly, following your healthcare provider's advice, and participating in public awareness campaigns.
Frequently Asked Questions
- What is antibiotic resistance?
Antibiotic resistance occurs when bacteria evolve and develop the ability to survive exposure to medications that previously killed them or inhibited their growth. This means that common infections can become harder to treat, leading to prolonged illness and increased healthcare costs.
- How do bacteria become resistant to antibiotics?
Bacteria can become resistant through various mechanisms, including genetic mutations and horizontal gene transfer, where they acquire resistance traits from other bacteria. Overuse and misuse of antibiotics in healthcare and agriculture also accelerate this process.
- What role do biofilms play in antibiotic resistance?
Biofilms are clusters of bacteria that adhere to surfaces and are encased in a protective layer. They can be incredibly resilient, making infections difficult to treat because antibiotics often fail to penetrate the biofilm effectively, allowing the bacteria to persist and thrive.
- What are the environmental factors contributing to antibiotic resistance?
Environmental factors such as pollution, improper waste management, and the use of antibiotics in agriculture can contribute to antibiotic resistance. These factors create conditions that promote the survival and spread of resistant bacteria in the environment.
- What are the global health implications of antibiotic resistance?
The rise of antibiotic-resistant bacteria poses significant challenges to global health, leading to increased morbidity, mortality, and healthcare costs. It threatens the effectiveness of surgeries, chemotherapy, and other medical treatments, making it a pressing public health issue.
- How can we combat antibiotic resistance?
Combating antibiotic resistance requires a multifaceted approach, including improved surveillance of resistance patterns, antibiotic stewardship programs to promote the responsible use of antibiotics, and public awareness campaigns to educate people about the risks of misuse.
- What can individuals do to help prevent antibiotic resistance?
Individuals can help prevent antibiotic resistance by using antibiotics only when prescribed by a healthcare professional, completing the full course of treatment, and never sharing antibiotics with others. Additionally, practicing good hygiene and vaccination can reduce the spread of infections.