The Future of Personalized Medicine and Technology
The world of medicine is evolving at a breakneck speed, and at the forefront of this revolution is personalized medicine. Imagine a healthcare system where treatments are tailored specifically to your genetic makeup, lifestyle, and environment. Sounds like something out of a sci-fi movie, right? But this is the reality we're stepping into. With advancements in technology, particularly in genetic testing and artificial intelligence, the future of healthcare is not just about treating diseases; it's about understanding each patient as a unique individual.
At its core, personalized medicine aims to provide the right treatment to the right patient at the right time. This approach is shifting the paradigm from a one-size-fits-all model to a more nuanced understanding of health and disease. As we delve deeper into the intricacies of our genetic code, we unlock the potential to predict health risks and tailor interventions accordingly. For instance, a patient with a specific genetic marker might respond better to one medication over another, significantly improving treatment outcomes. This is not just a dream; it’s happening now, and it’s set to expand exponentially in the coming years.
Furthermore, the integration of technology into personalized medicine is nothing short of revolutionary. The fusion of big data, artificial intelligence, and genomics is creating a robust framework for understanding complex health issues. Imagine having a healthcare system that can analyze millions of data points in seconds to determine the most effective treatment for you. This is the power of technology in medicine, and it’s changing how we approach healthcare at every level.
However, with great power comes great responsibility. As we embrace these advancements, we must also navigate the challenges they present. Ethical considerations, such as data privacy and equitable access to personalized treatments, are critical. How do we ensure that sensitive genetic information is protected? How do we make sure that these groundbreaking treatments are accessible to everyone, not just a privileged few? These are the questions we must grapple with as we forge ahead into this exciting new era of healthcare.
In summary, the future of personalized medicine is bright, filled with promise and potential. As we continue to harness the power of technology and deepen our understanding of human genetics, we are not just treating diseases; we are redefining what it means to be healthy. The journey ahead may be fraught with challenges, but the rewards—enhanced patient care, improved treatment outcomes, and a more personalized approach to health—are well worth the effort.
- What is personalized medicine? Personalized medicine is an innovative approach to healthcare that tailors treatment strategies to the individual characteristics of each patient, including their genetic makeup.
- How does technology play a role in personalized medicine? Technology, particularly in the fields of genetic testing and artificial intelligence, enhances our ability to analyze data and tailor treatments to individual patients.
- What ethical concerns are associated with personalized medicine? Key ethical concerns include data privacy, consent, and ensuring equitable access to advanced treatments for all patients.
- What are the benefits of personalized medicine? The primary benefits include improved treatment efficacy, reduced adverse effects, and a more proactive approach to disease prevention.

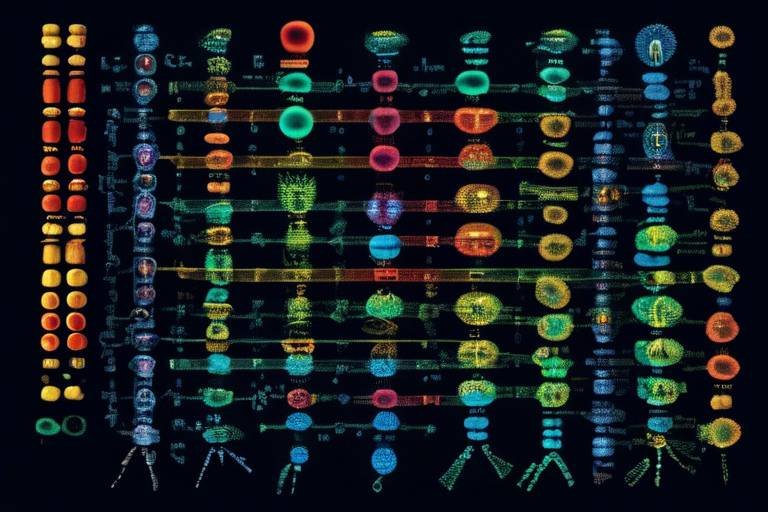
Advancements in Genetic Testing
Genetic testing is truly a game-changer in the realm of personalized medicine. Imagine being able to tailor treatments specifically to your genetic makeup—sounds like something out of a sci-fi movie, right? But it's happening now! With the rapid advancements in genomics, healthcare providers can identify genetic predispositions to various diseases, allowing for **proactive** rather than reactive healthcare. This means that instead of waiting for symptoms to appear, doctors can take preventive measures based on an individual's unique genetic profile.
One of the most exciting aspects of genetic testing is its ability to influence disease prevention and management strategies. For instance, if you have a family history of breast cancer, genetic tests can determine if you carry the BRCA1 or BRCA2 gene mutations. Armed with this knowledge, you and your healthcare provider can discuss options ranging from increased surveillance to preventive surgeries. This is not just about treatment; it’s about empowering patients to make informed decisions about their health.
Furthermore, the integration of genetic testing into routine medical care is becoming more common. Many healthcare systems are now offering genetic screenings as part of standard check-ups. This shift is crucial because it normalizes the conversation around genetics and health, making it less of a niche topic and more of a standard practice. The earlier we can identify risks, the better we can manage them. Think of it as having a roadmap for your health journey—one that highlights potential hazards along the way.
However, it’s essential to recognize that with great power comes great responsibility. The rise of genetic testing also brings forth a plethora of ethical considerations. For instance, how do we ensure that this sensitive information is kept secure? And what about the implications of genetic discrimination by employers or insurance companies? These are questions that need to be addressed as we embrace the future of personalized medicine.
Moreover, genetic testing is not just limited to hereditary diseases. Recent advancements have expanded the scope to include pharmacogenomics, which studies how genes affect a person’s response to drugs. This means that medications can be customized based on an individual's genetic profile, potentially reducing adverse drug reactions and increasing the effectiveness of treatments. Imagine a world where your medication is tailored to work with your body, rather than against it—this is the promise of pharmacogenomics!
As we look ahead, it's clear that the future of genetic testing is bright. Innovations such as next-generation sequencing (NGS) are making tests faster, cheaper, and more accessible than ever before. This technology allows for the simultaneous sequencing of millions of DNA fragments, providing a comprehensive view of an individual's genetic makeup. The implications for personalized medicine are profound, as healthcare providers will have an unprecedented amount of data at their fingertips.
In conclusion, the advancements in genetic testing are paving the way for a new era in healthcare. By allowing for more personalized and proactive treatment options, we can improve patient outcomes and enhance the overall quality of care. However, as we embrace these advancements, we must also navigate the ethical landscape to ensure that everyone can benefit from the incredible potential of personalized medicine.
- What is genetic testing? Genetic testing involves analyzing DNA to identify genetic variations that may indicate a predisposition to certain diseases or conditions.
- How can genetic testing influence treatment? It allows healthcare providers to tailor treatments based on an individual's genetic profile, improving effectiveness and reducing adverse reactions.
- Are there ethical concerns with genetic testing? Yes, issues such as data privacy, potential discrimination, and informed consent are significant considerations in the field.
- What is pharmacogenomics? Pharmacogenomics is the study of how genes affect a person's response to drugs, enabling personalized medication plans.

Artificial Intelligence in Healthcare
Artificial Intelligence (AI) is not just a buzzword; it’s a game-changer in the healthcare industry. Imagine a world where diagnoses are quicker, treatments are more precise, and patient care is significantly enhanced—all thanks to AI technologies. This transformation is not merely theoretical; it's happening right now, and it's reshaping the way we think about health and wellness. The integration of AI into healthcare systems is enabling providers to harness the power of data like never before. With vast amounts of health information being generated daily, AI is stepping in to analyze this data, offering insights that can lead to better patient outcomes.
One of the most exciting aspects of AI in healthcare is its ability to enhance diagnostic accuracy. Traditional diagnostic methods, while effective, can sometimes be limited by human error or bias. AI algorithms, on the other hand, can analyze imaging data, lab results, and patient histories with incredible precision. For example, AI tools can identify patterns in medical images that may go unnoticed by the human eye, leading to earlier and more accurate diagnoses of conditions like cancer or heart disease. This capability not only improves patient care but also streamlines the workflow for healthcare providers, allowing them to focus more on patient interaction and less on administrative tasks.
Moreover, AI is instrumental in personalizing treatment plans. By analyzing a patient’s genetic makeup, lifestyle, and preferences, AI can suggest tailored therapies that are more likely to be effective. This is particularly important in fields like oncology, where treatments can vary significantly between individuals. The use of AI in this context can be likened to having a personal coach who knows your strengths and weaknesses, guiding you towards the most effective path to recovery.
At the heart of AI’s success in healthcare are machine learning algorithms. These algorithms are designed to learn from data, improving their accuracy over time. They can sift through enormous datasets, identifying trends and predicting patient responses to specific therapies. For instance, a machine learning model might analyze thousands of patient records to determine which treatment protocols yield the best outcomes for particular demographics. This predictive power is invaluable, as it allows healthcare providers to make informed decisions that enhance the quality of care.
Predictive analytics is another facet of AI that holds tremendous potential for personalized medicine. By utilizing historical data, predictive analytics can forecast health outcomes, helping providers to craft individualized treatment plans. For example, if a patient has a family history of diabetes, predictive analytics can alert healthcare providers to monitor that patient more closely. This proactive approach not only improves individual care but also aids in the prevention of diseases on a larger scale.
Natural Language Processing (NLP) is yet another AI application that enhances communication between patients and providers. NLP technology can analyze unstructured data, such as doctor’s notes and patient feedback, to extract meaningful insights. Imagine a scenario where a doctor can quickly review a patient’s entire history through a simple voice command, thanks to NLP. This capability not only saves time but also ensures that healthcare providers have a comprehensive view of their patients’ needs, leading to better-informed decisions.
As we delve deeper into the realm of AI in healthcare, it’s essential to acknowledge both the benefits and the challenges that come with these advancements. While AI offers unparalleled opportunities for improving patient care, it also raises questions about data privacy and ethical considerations. The journey towards fully integrating AI into healthcare is ongoing, but the potential it holds for personalized medicine is truly exciting.
- What is AI in healthcare? AI in healthcare refers to the use of artificial intelligence technologies to analyze data and improve patient care.
- How does AI enhance diagnostic accuracy? AI analyzes medical imaging and patient data to identify patterns that may be missed by human providers.
- What role do machine learning algorithms play in personalized medicine? Machine learning algorithms analyze vast datasets to predict patient responses and optimize treatment plans.
- What is predictive analytics in healthcare? Predictive analytics uses historical data to forecast health outcomes and guide treatment decisions.

Machine Learning Algorithms
Machine learning algorithms are at the forefront of revolutionizing healthcare, especially in the realm of personalized medicine. Imagine having a tool that can sift through mountains of medical data, identifying patterns and predicting outcomes faster than any human could. That’s the power of machine learning! These algorithms analyze vast datasets, which include everything from genetic information to treatment histories, enabling healthcare professionals to tailor treatments to individual patients. This capability not only enhances the accuracy of diagnoses but also significantly improves treatment personalization.
One of the most exciting aspects of machine learning in healthcare is its ability to predict patient responses to specific therapies. For instance, algorithms can analyze previous patient data to determine which treatments have been most effective for individuals with similar genetic backgrounds or health conditions. This predictive capability is akin to having a personalized health crystal ball, allowing doctors to make informed decisions that are tailored to each patient's unique profile.
To better understand how machine learning algorithms function in the context of personalized medicine, let’s break it down into a few key areas:
- Data Collection: Machine learning requires vast amounts of data to learn and make predictions. This data can come from electronic health records, clinical trials, and even wearable health devices.
- Algorithm Training: Once the data is collected, algorithms are trained to recognize patterns. This training involves adjusting the algorithm's parameters until it can accurately predict outcomes based on the input data.
- Real-Time Analysis: After training, these algorithms can analyze new patient data in real-time, providing immediate insights that can guide treatment decisions.
Moreover, the integration of machine learning with other technologies, such as genomics and imaging, creates a powerful synergy that enhances the precision of medical interventions. For example, a machine learning algorithm might analyze genetic data alongside imaging results to help oncologists determine the most effective course of action for cancer patients. This multi-faceted approach not only improves the chances of successful treatment but also minimizes the risk of adverse side effects.
However, it’s essential to acknowledge that while machine learning holds immense potential, it also poses challenges. The algorithms are only as good as the data fed into them; biased or incomplete data can lead to inaccurate predictions. Therefore, ongoing efforts to improve data quality and algorithm transparency are crucial. As we look to the future, the collaboration between healthcare professionals and data scientists will be vital in refining these algorithms, ensuring they are both effective and equitable in their applications.
In summary, machine learning algorithms are transforming the landscape of personalized medicine. By harnessing the power of data, these algorithms enable healthcare providers to make informed, individualized treatment decisions, ultimately leading to better patient outcomes. The journey is just beginning, and as technology continues to evolve, the possibilities for enhancing healthcare through machine learning are boundless.

Predictive Analytics
Predictive analytics is a game-changer in the realm of personalized medicine. Imagine having the ability to foresee health outcomes before they even manifest; it’s like having a crystal ball for healthcare! By leveraging historical data and advanced statistical algorithms, predictive analytics allows healthcare providers to make informed decisions tailored to individual patients. This approach not only enhances the accuracy of diagnoses but also optimizes treatment plans, ensuring that patients receive the most effective interventions based on their unique genetic makeup and health history.
The essence of predictive analytics lies in its capacity to analyze vast amounts of data, identifying patterns and trends that might otherwise go unnoticed. For instance, by examining data from previous patients, algorithms can predict how a new patient might respond to a specific treatment. This is particularly vital in fields like oncology, where treatments can vary significantly in effectiveness from one patient to another. By anticipating how a patient will respond, doctors can customize their treatment plans, potentially improving outcomes and minimizing adverse effects.
Moreover, predictive analytics can play a crucial role in preventive care. By identifying individuals at high risk for certain conditions, healthcare providers can implement early interventions. This proactive approach not only improves patient outcomes but can also reduce overall healthcare costs. For example, if predictive models indicate that a patient is at a higher risk of developing diabetes, lifestyle changes and regular monitoring can be initiated to mitigate that risk.
To illustrate the impact of predictive analytics, consider the following table that highlights its applications across different medical fields:
| Medical Field | Application | Benefits |
|---|---|---|
| Oncology | Predicting treatment responses | Customized treatment plans |
| Cardiology | Identifying heart disease risk | Early intervention and prevention |
| Neurology | Forecasting progression of neurological disorders | Tailored management strategies |
| Diabetes Care | Risk assessment for complications | Preventative measures and lifestyle changes |
As we move forward, the integration of predictive analytics into healthcare practices will likely continue to expand. The potential for improved patient outcomes is significant, but it also raises questions about data accuracy and the ethical implications of using such sensitive information. It is essential for healthcare providers to ensure that predictive models are not only accurate but also equitable, providing benefits to all patients regardless of their background.
In conclusion, predictive analytics stands at the forefront of personalized medicine, offering unprecedented opportunities to enhance patient care. By predicting health outcomes and tailoring treatments accordingly, we are not just treating diseases; we are paving the way for a future where healthcare is as unique as the individuals it serves.
- What is predictive analytics in healthcare?
Predictive analytics in healthcare refers to the use of data analysis techniques to predict future health outcomes based on historical data. It enables healthcare providers to tailor treatments and interventions to individual patients. - How does predictive analytics improve patient care?
By predicting potential health issues and treatment responses, predictive analytics allows for personalized treatment plans that can lead to better health outcomes and more efficient use of healthcare resources. - Are there ethical concerns with predictive analytics?
Yes, ethical concerns include data privacy, consent for data use, and ensuring equitable access to predictive technologies across different patient demographics.

Natural Language Processing
Natural Language Processing (NLP) is a game-changer in the realm of personalized medicine, acting as a bridge between human communication and machine understanding. Imagine having a personal assistant that not only understands your health concerns but can also interpret complex medical jargon and translate it into plain language. This is precisely what NLP does! By leveraging algorithms that can analyze and comprehend human language, NLP enhances the interaction between patients and healthcare providers, ensuring that critical information is conveyed accurately and efficiently.
One of the most significant benefits of NLP in personalized medicine is its ability to process unstructured data, such as clinical notes, patient feedback, and research articles. Traditional data analysis often struggles with this type of information, but NLP can sift through mountains of text to extract valuable insights. For instance, NLP can identify trends in patient symptoms or treatment responses that might not be apparent through structured data alone. This capability allows healthcare professionals to tailor treatment plans based on real-world patient experiences, leading to more effective outcomes.
Furthermore, NLP can facilitate better patient-provider communication. How often have you left a doctor's appointment feeling confused about your diagnosis or treatment plan? With NLP tools, patients can receive clear explanations and follow-up information in a format that is easy to understand. Imagine receiving a personalized summary of your visit via text or email, highlighting key points discussed, recommended actions, and even links to additional resources. This not only empowers patients but also encourages active participation in their own healthcare journey.
Moreover, NLP can assist in the development of chatbots and virtual health assistants, providing patients with immediate responses to their inquiries. These AI-driven tools can handle a variety of tasks, from scheduling appointments to answering frequently asked questions about medications. They can also triage symptoms, directing patients to the appropriate care level based on their reported issues. This is particularly beneficial in managing chronic diseases where timely intervention is crucial.
However, while the potential of NLP in personalized medicine is immense, it is essential to address some challenges. One significant concern is the accuracy of the algorithms used. If NLP systems misinterpret a patient's input, it could lead to incorrect conclusions or recommendations. Continuous training and refinement of these systems are necessary to ensure they remain reliable and effective. Additionally, there are ethical considerations regarding data privacy and security, as NLP systems often require access to sensitive patient information.
To summarize, Natural Language Processing is revolutionizing personalized medicine by enhancing communication, improving data analysis, and facilitating patient engagement. As technology continues to evolve, we can expect NLP to play an even more prominent role in shaping the future of healthcare, making it more accessible and tailored to individual needs.
- What is Natural Language Processing (NLP)?
NLP is a branch of artificial intelligence that focuses on the interaction between computers and humans through natural language. It enables machines to understand, interpret, and respond to human language in a valuable way. - How does NLP improve patient care?
NLP enhances patient care by facilitating better communication between patients and healthcare providers, allowing for personalized treatment plans based on real-world data, and providing immediate responses to patient inquiries through AI-driven tools. - Are there any risks associated with using NLP in healthcare?
Yes, there are risks such as data privacy concerns and the potential for misinterpretation of patient input, which can lead to incorrect recommendations. Continuous training and ethical considerations are crucial to mitigate these risks.

Telemedicine and Remote Monitoring
In today's fast-paced world, telemedicine has emerged as a game-changer in the healthcare landscape, providing patients with unprecedented access to personalized care. Imagine being able to consult with your doctor from the comfort of your home, without the hassle of waiting rooms or long commutes. This is not just a dream; it's a reality made possible by advancements in technology. Telemedicine allows healthcare providers to deliver care remotely, utilizing video calls, mobile apps, and other digital platforms. This convenience is particularly beneficial for those managing chronic conditions, as it enables continuous monitoring and timely interventions.
Remote monitoring technologies are at the forefront of this transformation. Devices such as wearable health trackers, smartwatches, and mobile health applications collect real-time data on patients' vital signs, activity levels, and even medication adherence. This data is then transmitted to healthcare professionals, who can analyze it to make informed decisions regarding treatment plans. For instance, a patient with diabetes can use a continuous glucose monitor that sends readings directly to their healthcare provider, allowing for immediate adjustments in insulin dosage if necessary. This proactive approach not only enhances patient outcomes but also fosters a stronger doctor-patient relationship, as patients feel more engaged in their own care.
However, the integration of telemedicine and remote monitoring is not without its challenges. While the benefits are clear, issues such as technology access and digital literacy can create barriers for certain populations. For instance, older adults or those living in rural areas may struggle with the technology required to access telehealth services. Additionally, concerns about data security and privacy are paramount, as sensitive health information is transmitted over digital platforms. It is crucial for healthcare organizations to implement robust security measures to protect patient data and build trust in these technologies.
Despite these challenges, the potential of telemedicine and remote monitoring to revolutionize personalized care is immense. As we continue to embrace these technologies, we must also prioritize education and accessibility to ensure that everyone can benefit from the advancements in healthcare. The future of medicine is not just about treating illnesses; it’s about empowering patients to take charge of their health, and telemedicine is leading the charge.
| Benefits of Telemedicine | Challenges of Telemedicine |
|---|---|
| Increased accessibility to healthcare | Technology access issues |
| Convenience and time-saving | Digital literacy requirements |
| Continuous monitoring of chronic conditions | Data security and privacy concerns |
| Improved patient engagement | Resistance to change from traditional methods |
As we look to the future, it is essential to embrace the innovations that telemedicine and remote monitoring bring to personalized medicine. By addressing the challenges head-on and ensuring equitable access, we can pave the way for a healthier society where everyone has the opportunity to receive the best possible care.
- What is telemedicine? Telemedicine refers to the use of technology to provide healthcare services remotely, allowing patients to consult with healthcare providers without needing to visit a clinic or hospital.
- How does remote monitoring work? Remote monitoring involves using devices that track health metrics, such as heart rate or blood sugar levels, and send this data to healthcare providers for analysis and recommendations.
- What are the benefits of telemedicine? Benefits include increased accessibility, convenience, continuous monitoring of chronic conditions, and improved patient engagement.
- Are there any challenges associated with telemedicine? Yes, challenges include technology access issues, digital literacy requirements, and concerns about data security and privacy.

Ethical Considerations in Personalized Medicine
As the field of personalized medicine continues to grow and evolve, it brings with it a host of ethical considerations that cannot be overlooked. With the ability to tailor treatments based on an individual's genetic makeup, lifestyle, and environment, the potential for improved patient outcomes is tremendous. However, this innovation also raises significant questions regarding privacy, consent, and equitable access to these advanced therapies.
One of the most pressing issues is data privacy and security. As healthcare providers collect and analyze vast amounts of personal data to create tailored treatment plans, the risk of data breaches and unauthorized access increases. Patients must trust that their sensitive information is being handled responsibly. In fact, a recent survey indicated that over 70% of individuals are concerned about how their data will be used and shared. To address these concerns, healthcare organizations must implement robust security measures and transparent data usage policies.
Furthermore, the question of informed consent becomes increasingly complex in personalized medicine. Patients should be fully aware of what their genetic data entails and how it will influence their treatment. This means that healthcare providers must not only explain the benefits of personalized medicine but also the potential risks and implications of genetic testing. It’s crucial for patients to feel empowered to make informed decisions about their healthcare, which can be challenging in a rapidly evolving field.
Equity in healthcare access is another critical ethical consideration. While personalized medicine holds great promise, it also risks widening the gap between those who can afford advanced treatments and those who cannot. Disparities in access to genetic testing and personalized therapies can lead to unequal health outcomes. To combat this, stakeholders in the healthcare system must work collaboratively to develop strategies that ensure all patients, regardless of their socioeconomic status, can benefit from these innovations. This may involve policy changes, funding for underserved populations, and increasing awareness about the importance of equitable access.
In conclusion, as we embrace the future of personalized medicine, it is essential to address these ethical considerations head-on. By prioritizing data privacy, ensuring informed consent, and advocating for equitable access, we can harness the power of personalized medicine while safeguarding the rights and well-being of all patients.
- What is personalized medicine?
Personalized medicine is a medical model that tailors healthcare treatments to individual characteristics, such as genetic makeup, lifestyle, and environment. - Why is data privacy important in personalized medicine?
Data privacy is crucial because personalized medicine relies on sensitive patient information. Protecting this data helps maintain trust between patients and healthcare providers. - How can we ensure equitable access to personalized medicine?
Ensuring equitable access involves policy changes, funding for underserved communities, and raising awareness about the importance of these treatments.

Data Privacy and Security
In the rapidly evolving field of personalized medicine, have emerged as paramount concerns. With the integration of advanced technologies, healthcare providers are now able to collect and analyze vast amounts of personal health data. This data, while essential for tailoring treatments and improving patient outcomes, also presents significant risks if not properly managed. Imagine your health information being as accessible as your favorite playlist; it sounds convenient, but it also raises a few eyebrows, right?
First and foremost, the challenge lies in ensuring that patient data is protected from unauthorized access. Cybersecurity threats are on the rise, and healthcare systems are prime targets. A breach can lead to sensitive information being exposed, which can have devastating consequences for patients. In fact, studies have shown that healthcare data breaches can have long-lasting effects on individuals, from identity theft to emotional distress. Consequently, healthcare organizations must adopt stringent security measures to safeguard this information.
Moreover, it's not just about protecting data from external threats; it's also about maintaining patient trust. Patients are more likely to share their genetic and health information if they believe it will be handled with care. This is where the concept of informed consent comes into play. Patients should be fully aware of how their data will be used, who will have access to it, and the potential risks involved. A clear and concise privacy policy can help bridge this gap, but it must be communicated effectively to ensure that patients feel comfortable.
To illustrate the importance of data privacy, consider the following table that outlines some of the key elements of a robust data security framework:
| Security Element | Description |
|---|---|
| Encryption | Encoding data to prevent unauthorized access. |
| Access Control | Restricting access to sensitive information to authorized personnel only. |
| Regular Audits | Conducting periodic reviews to identify vulnerabilities and ensure compliance. |
| Data Anonymization | Removing identifiable information to protect patient identity. |
Furthermore, as technology continues to advance, the ethical implications surrounding data usage become even more complex. For instance, the potential for data misuse raises questions about who owns the data and how it can be utilized. Are patients merely subjects in a vast experiment, or do they have a say in how their information is leveraged? These questions highlight the need for ongoing dialogue between healthcare providers, patients, and policymakers to establish clear guidelines that prioritize patient rights.
In conclusion, while personalized medicine holds incredible promise for improving patient care, it is crucial to address the challenges that accompany it. By implementing robust security measures, fostering transparent communication, and engaging patients in discussions about their data, we can create a healthcare environment that not only innovates but also respects and protects the individuals it serves.
- What is personalized medicine? Personalized medicine is a medical model that tailors treatment to the individual characteristics of each patient, often utilizing genetic or other biomarker information.
- Why is data privacy important in healthcare? Data privacy is crucial because it protects sensitive patient information from unauthorized access, ensuring trust between patients and healthcare providers.
- How can patients ensure their data is secure? Patients can ensure data security by asking healthcare providers about their privacy policies, understanding how their data will be used, and being aware of their rights regarding data access and sharing.
- What are the consequences of a data breach in healthcare? Consequences can include identity theft, loss of patient trust, and legal ramifications for healthcare organizations.

Equity in Healthcare Access
In the ever-evolving landscape of personalized medicine, stands as a crucial pillar. As we embrace cutting-edge technologies and tailored treatments, we must also confront the stark reality that not everyone has equal access to these advancements. Imagine a world where a life-saving genetic therapy is available, but only to those who can afford it. This scenario is not just hypothetical; it’s a pressing issue that demands our attention. The disparities in healthcare access can be attributed to various factors, including socioeconomic status, geographic location, and systemic biases that have lingered for decades.
To truly harness the benefits of personalized medicine, we need to address these inequities head-on. One of the primary challenges is the digital divide, where individuals in rural areas or low-income communities lack access to the necessary technology and internet connectivity to benefit from telemedicine and remote monitoring. Furthermore, even when advanced treatments are available, the cost can be prohibitive, leaving many patients in a lurch. According to recent studies, nearly 30% of patients report that they have had to forgo necessary treatments due to financial constraints. This statistic is alarming and highlights the need for systemic change.
Moreover, we must consider the importance of cultural competency in healthcare. Providers must be equipped to understand and respect the diverse backgrounds of their patients to ensure that personalized medicine is truly beneficial for everyone. This means not only providing language support but also being aware of cultural beliefs and practices that may influence a patient's approach to healthcare. A one-size-fits-all model simply does not work in medicine; we need to customize our approach to fit the unique needs of each community.
Another significant aspect is the role of policy in shaping equitable access to healthcare. Governments and healthcare organizations must collaborate to create policies that promote affordable access to personalized medicine. This can include funding for research that focuses on underserved populations, subsidies for treatments, and initiatives that increase awareness about available healthcare resources. By addressing these issues, we can pave the way for a more equitable healthcare system where everyone has the opportunity to benefit from the latest advancements in medical science.
In conclusion, equity in healthcare access is not just a moral obligation; it is essential for the success of personalized medicine. As we continue to innovate and develop new treatments, we must ensure that these advancements are accessible to all, regardless of their background or circumstances. Only then can we truly claim to be making progress in the field of medicine. Addressing these disparities requires a concerted effort from all stakeholders—healthcare providers, policymakers, and patients alike. Together, we can create a healthcare system that is inclusive and equitable for everyone.
- What is personalized medicine? Personalized medicine is an innovative approach to healthcare that tailors treatment and prevention strategies to individual patient characteristics, including genetics, environment, and lifestyle.
- Why is equity in healthcare access important? Equity in healthcare access ensures that all individuals, regardless of their background or financial status, can benefit from advancements in medical technology and treatments, leading to better health outcomes for everyone.
- How can we improve access to personalized medicine? Improving access can be achieved through policy changes, increased funding for underserved communities, and enhancing digital infrastructure to support telemedicine and remote monitoring.
Frequently Asked Questions
- What is personalized medicine?
Personalized medicine refers to tailoring medical treatment to the individual characteristics of each patient. This approach takes into account factors like genetics, environment, and lifestyle, allowing for more effective and targeted therapies.
- How does genetic testing contribute to personalized medicine?
Genetic testing plays a crucial role in personalized medicine by identifying specific genetic markers associated with diseases. This information helps healthcare providers develop customized treatment plans that are more effective for each individual, enhancing disease prevention and management.
- What role does artificial intelligence play in healthcare?
Artificial Intelligence (AI) enhances healthcare by analyzing vast amounts of data to provide insights that improve diagnostic accuracy and treatment personalization. AI algorithms can identify patterns in patient data, helping doctors make informed decisions about patient care.
- What are machine learning algorithms, and how are they used?
Machine learning algorithms are a subset of AI that learn from data to make predictions. In healthcare, they analyze historical patient data to predict how individuals might respond to specific therapies, allowing for more tailored treatment plans.
- What is predictive analytics in personalized medicine?
Predictive analytics uses historical health data to forecast future health outcomes. This technique is vital for creating personalized treatment plans, as it helps healthcare providers anticipate how patients might respond to different interventions.
- How does Natural Language Processing (NLP) enhance personalized medicine?
NLP improves communication between patients and healthcare providers by interpreting and analyzing patient data more effectively. It helps in understanding patient histories and preferences, which can lead to better personalized treatment strategies.
- What are the benefits of telemedicine in personalized care?
Telemedicine increases access to personalized healthcare by allowing patients to consult with providers remotely. This is particularly beneficial for managing chronic diseases, as it offers convenience and continuous monitoring without the need for in-person visits.
- What ethical concerns arise with personalized medicine?
The rise of personalized medicine raises several ethical issues, including privacy concerns about patient data, the need for informed consent, and ensuring equitable access to advanced treatments for all patients, regardless of their socioeconomic status.
- How important is data privacy in personalized medicine?
Data privacy is crucial in personalized medicine as it involves sensitive patient information. Safeguarding this data is essential to maintain trust between patients and healthcare providers, especially with the increasing reliance on digital health technologies.
- What strategies can ensure equity in healthcare access?
To promote equity in healthcare access, strategies such as improving healthcare infrastructure in underserved areas, offering financial assistance, and implementing policies that address disparities in treatment availability are essential. This ensures that all patients can benefit from advancements in personalized medicine.